In the US, about 40% of adults will face sciatica’s sharp, lasting pain sometime in their lives. This places sciatica as a top reason for chronic pain issues across the country. The causes of Sciatica, or Lumbar Radiculopathy, involve many factors that can harm a person’s spinal health and everyday life.
Sciatica is more than just brief pain. It’s a major health problem, rooted in both how we live and our body’s structure. We must work on ways to prevent sciatica, understanding both lifestyle and biological reasons behind back pain.
To really grasp sciatica’s effects, we need to look at how back pain starts. This includes everything from sudden injuries to long-term wear and tear. We must tackle Lumbar Radiculopathy’s causes in our journey to better manage chronic pain. This will help lessen sciatica’s heavy toll on those it affects.
Key Takeaways
- Sciatica affects up to 40% of adults, underscoring its significance in chronic pain management.
- A multifaceted approach to understanding Sciatica causes is crucial for effective treatment.
- Lumbar Radiculopathy triggers range from lifestyle factors to anatomical changes, impacting spinal health.
- Back pain origins are diverse, necessitating personalized sciatica prevention strategies.
- Educating about sciatica’s prevalence and impact is essential for enhancing patient quality of life.
What is Sciatica?
Sciatica is known for its intense leg pain which often signals deeper chronic back issues. This pain moves along the sciatic nerve’s path. It goes from the lower back down each leg. Sciatica nerve pain can feel drastically different, ranging from sharp pain to a gentle tingling.
People with sciatica often feel sciatica symptoms like pain, numbness, and muscle weakness. These can greatly disrupt daily life. Simple movements or anything that pressures the lower spine might become difficult.
Patients frequently describe sciatica symptoms as ‘a pain that shoots down the leg,’ which can be incapacitating at its peak intensity.
It’s vital to understand sciatica to find effective treatments and handle recurring lower back pain. This is a key sign of sciatica.
- Sharp, shooting pain observable from the lower back to below the knee
- Numbness or tingling in the legs and feet
- Muscle weakness affecting leg mobility
The onset of sciatica may happen slowly or suddenly. It’s important to know about its causes. Knowing the lifestyle or physical strains linked to sciatica is essential. This awareness can help prevent this painful condition.
Demystifying Lumbar Radiculopathy
Lumbar Radiculopathy, or Sciatica, involves complex medical terms that confuse many. We aim to make the conditions like nerve root irritation, spinal nerve compression, and radicular pain easier to understand. These terms are key to explaining Sciatica.
At its core, Sciatica comes from spinal nerve compression or irritation in the spine’s lumbar segment. This issue causes nerve root irritation leading to radicular pain. The pain typically spreads from the lower back to the legs along the sciatic nerve. Knowing these terms helps in finding the right treatment.
The below table shows how spinal nerve compression and nerve root irritation are connected to patient symptoms:
| Condition | Description | Implications for Radicular Pain |
|---|---|---|
| Spinal Nerve Compression | Occurs when spinal structures press into spaces meant for spinal nerves. This often happens due to spinal stenosis or herniated disc. | This pressure causes intense, sharp pain along the nerve’s path. |
| Nerve Root Irritation | Is caused by inflammation from disc issues or external pressure on nerve roots. | Leads to a burning or tingling downward sensation, affecting leg movement and comfort. |
Getting to know these conditions through Sciatica clarification helps clear up misconceptions. It also prepares those suffering to seek treatment with a clear understanding of their condition.
The Anatomy of Sciatica
Understanding the sciatic nerve anatomy is key to knowing why sciatica happens. This nerve is the body’s largest, starting from the lumbar spine structure. It runs through the hip and down each leg. When we talk about radicular symptoms, the path of the sciatic nerve matters a lot. Its path makes it likely to get irritated or compressed, causing severe nerve pain.
The role of nerve pain pathways in sciatica is vital. These pathways carry pain signals from the spinal cord to the brain. If the sciatic nerve gets pinched or irritated in the lower back, it sends pain signals. These signals are known as radicular symptoms. They cause pain, numbness, or tingling in the legs.
| Lumbar Spine Structure | Impact on Sciatic Nerve |
|---|---|
| L1-L5 Vertebrae | Direct formation of sciatic nerve roots |
| Intervertebral Discs | Potential source of nerve compression |
| Sacral Plexus Location | Site where sciatic nerve converges and exits spine |
Knowing a lot about the lumbar spine structure helps doctors diagnose and treat sciatica well. Herniated discs often lead to sciatic nerve compression. This shows how connected spinal anatomy and nerve issues are. Spotting radicular symptoms early can greatly help in managing sciatic nerve pain. It highlights the need for a full approach to understand and treat this issue.
Understanding Sciatica (Lumbar Radiculopathy)
Getting to know the cause of Sciatica and lumbar disc issues is vital. It helps in dealing effectively with this painful state. Sciatica usually points to lumbar radiculopathy, where spinal problems lead to nerve pain. This pain might spread from the lower back to the legs.
Exploring the causes of radiculopathy origins, we must look at many factors. These include anything that might press on or irritate the nerves. Herniated or bulging discs are often to blame. Thus, they are key in diagnosing and treating sciatic pain.
- Herniated Discs: When the soft material inside a disc leaks out, it can press on a nerve root, leading to the symptoms associated with sciatica.
- Osteophytes or Bone Spurs: These are bony growths that can form on vertebrae and potentially irritate nearby nerve roots, escalating lumbar disc issues.
- Spinal Stenosis: A narrowing of the spaces within the spine can place additional pressure on the nerves traveling through the spine.
The connection between these spine problems and sciatica pain is critical. It highlights the need to aim treatments at the root of nerve compression. This strategy is more effective than just addressing the symptoms.
| Condition | Description | Impact on Sciatica |
|---|---|---|
| Herniated Disc | Disc material pushes into the spinal canal, affecting nerve function. | Direct compression of nerve roots leading to Sciatica. |
| Bone Spurs | Overgrowth of bone on vertebrae, encroaching on nerve space. | Potentially irritates or compresses spinal nerves. |
| Spinal Stenosis | Narrowing of the spinal canal that houses the nerve roots. | Can lead to significant nerve pressure and manifest as sciatic pain. |
For a deeper dive into the cause of Sciatica, using diagnostic imaging is key. It gives a clear view of the spine to find the exact cause of pain. This knowledge helps in creating treatments that focus on the real issue, not just the pain.

Common Triggers of Sciatica
Sciatica is a harmful nerve issue. It can be caused by different spinal problems. Each one adds to the severe pain and discomfort of sciatica. Knowing these triggers—like disc herniation, spinal stenosis, and spondylolisthesis—is vital for diagnosis and managing sciatica.
Disc Herniation
Disc herniation is a frequent cause of sciatica. It happens when the disc’s inner core pushes out through the outer layer. This bulge can press on the sciatic nerve. It causes nerve root compression and radicular pain. This injury damages the disc and worsens pain by hurting surrounding tissues.
Spinal Stenosis
Spinal stenosis happens when the spine narrows. It puts too much pressure on nerves, including the sciatic nerve. Mainly in older adults, it results from aging. This aging leads to buildup of wear and tear, increasing chances of spinal and nerve root compression.
Spondylolisthesis
Spondylolisthesis is another major cause. It occurs when one vertebra slips over another. Often, it squeezes the nerve roots connected to the sciatic nerve. This slipping messes up the spine’s alignment and tightens nerve pathways. It makes back injuries and sciatica symptoms worse.
| Condition | Description | Impact on Sciatica |
|---|---|---|
| Disc Herniation | Bulging of disc material that presses on the sciatic nerve | Direct compression leading to acute pain |
| Spinal Stenosis | Narrowing of spinal canal, compressing spinal nerves | Increased spinal pressure causing chronic symptoms |
| Spondylolisthesis | Displacement of a vertebra over another | Nerve compression and misalignment leading to intensified pain |
Lifestyle and Sciatica Risk Factor
Our lifestyle and work habits have a big impact on our health, especially with conditions like sciatica. Being inactive or facing work-related risks are key factors for sciatica. This part talks about how not moving much and certain job conditions increase the risk of sciatica.
Sedentary Lifestyle
Not moving enough is a top reason for sciatica. This is because sitting a lot can hurt your posture and put more pressure on your spine, leading to back pain. Not moving makes it easier for the spinal discs to wear out, which is often linked to sciatica. It’s important to move around and use good workspace setups to prevent back pain.
Occupational Hazards
Getting injured at work can also lead to sciatica. This is especially true for jobs that make you do the same motions over and over or sit for too long. Knowing how to set up your workspace correctly can help lower the risk. Using chairs that support your back well and arranging your work area to encourage sitting upright are good ways to prevent sciatica caused by work habits.
| Factor | Description | Prevention Strategy |
|---|---|---|
| Physical Inactivity | Lack of movement leading to increased spinal pressure and poor posture. | Regular stretching, frequent breaks, ergonomic workplace design. |
| Workplace Injury | Repetitive strain or improper posture during long work hours. | Implement ergonomic furniture and posture training sessions. |

Physical Conditions that Precipitate Sciatica
Obesity and pregnancy are two common states that can deeply affect sciatica. These conditions lead to weight-induced nerve pressure. They also complicate health issues, especially during pregnancy. Knowing this, managing weight can help ease sciatic pain.
Pregnancy-Related Sciatica
Many expectant mothers face back pain. It affects their health and ability to move. The extra weight from pregnancy puts pressure on the spine, causing nerve compression. Managing this is key to easing pain and improving the pregnancy journey.
Obesity and Sciatica
For those not pregnant, being overweight is a big reason for sciatica. It puts pressure on the spine’s nerves. Having a tailored plan for weight management is crucial. It not only lessens pain but might also reverse some problems caused by sciatica.
| Condition | Impact on Spine | Recommended Management |
|---|---|---|
| Pregnancy | Increased load during later trimesters | Gentle exercise, maternity support belts |
| Obesity | Chronic pressure on lumbar spine | Weight loss through diet and exercise |
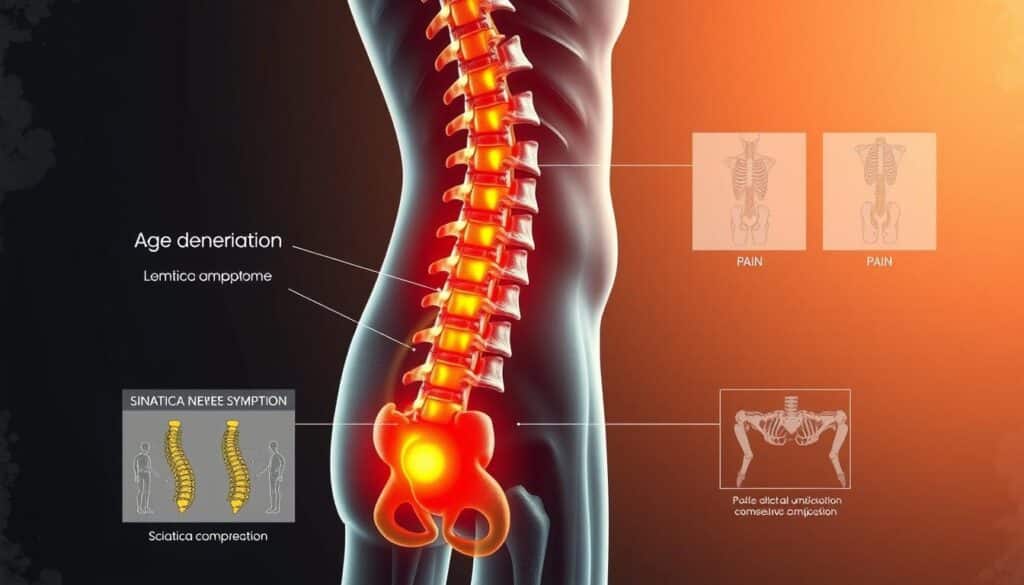
Age-Related Changes and Sciatica
As people get older, their spine changes in ways that may cause elderly back pain and age-related sciatic pain. The aging spine and degenerative disc disease play big roles in starting sciatica in seniors. It’s key to know how these issues lead to sciatica.
Spinal discs and joints break down over time. This is due to the discs losing moisture and stretchiness, known as degenerative disc disease. Such wear reduces their shock-absorbing ability. It may make vertebrae grind together, causing pain or even squeezing nerves. This is crucial in how sciatica symptoms start.
The aging spine might also deal with bone spurs and spinal stenosis. These conditions make the spaces where nerves travel smaller. Especially, they can press on the sciatic nerve root, starting age-related sciatic pain. Here’s a table that shows common spinal changes and their effects on the sciatic nerve.
| Spinal Change | Effect on Sciatica |
|---|---|
| Degenerative Disc Disease | Disc narrowing leading to nerve compression |
| Bone Spurs | Spurs can impinge directly on nerve roots |
| Spinal Stenosis | Narrowing of spinal canal pinching sciatic nerve |
| Arthritis | Inflammation and swelling impacting nerve function |
Dealing with aging spine risks and slowing degenerative disc disease demands action. Keeping a healthy weight and staying flexible are key. Such efforts can ease elderly back pain and cut the chance of getting sciatica.
Though spine changes with age can’t be stopped, knowing about them and taking preventive steps can protect back health and lessen sciatica’s effects in seniors. Regular visits to a doctor who knows about aging or spine care can give tailored advice for managing back issues.
Sciatica and Underlying Medical Conditions
Illnesses like diabetes can greatly affect nerve health, leading to problems like diabetes-related Sciatica. It’s key to see how health conditions and nerve damage, including sciatica pain, are linked.
Systemic diseases impact the whole body and involve blood vessels which keep nerves healthy, like the sciatic nerve. Diseases harming vascular health can lead to nerve issues. Diabetes can cause microvascular damage hurting nerve function, leading to Sciatica.
| Chronic Condition | Relationship to Nerve Health | Specific Impact on Sciatica |
|---|---|---|
| Diabetes | Causes microvascular damage that can lead to peripheral neuropathy. | Increase in diabetes-related Sciatica due to nerve inflammation and damage. |
| Hypertension | Can lead to blood vessel damage and reduced blood flow to nerves. | Potentially increases risk of nerve damage and subsequent Sciatica. |
| Lupus | Autoimmune inflammation can directly affect nerve tissue. | Might result in Sciatic nerve pain as a secondary complication. |
Knowing these links is crucial for Sciatica sufferers with a chronic illness. Proper care of systemic diseases might lower or prevent nerve damage leading to Sciatica. Thus, addressing these health problems is key to lessening sciatic pain and bettering life quality.
Understanding Nerve Compression and Injury
Nerve compression and trauma-induced back pain play big roles in sciatica related to injury. Knowing how nerve compression happens helps us understand the pain. It also shows us how to help nerves heal.
Injury-related sciatica comes from nerves being squeezed. This happens when bones, cartilage, or muscles put too much pressure on nerve roots from the spine. This pressure causes pain and can injure the nerve. If not treated, it could lead to ongoing problems.
Healing nerves takes time and sometimes we need to fix or adjust the body to help. How we recover depends on how bad the nerve damage is from the back pain. So, getting the right treatment plan is important.
| Condition | Symptoms | Recovery Strategies |
|---|---|---|
| Nerve Impingement | Persistent sharp pain, numbness, weakness | Physical therapy, anti-inflammatory medications |
| Trauma-Induced Back Pain | Acute back pain, reduced mobility | Cold/heat therapy, controlled physical activity |
| Injury-Related Sciatica | Radiating pain down the leg, discomfort when sitting | Steroid injections, surgery (if necessary) |
Treating nerve injuries might mean medical care and changing your lifestyle. It’s important to balance rest and exercises for healing. This helps in getting better from sciatica caused by injuries.

Are you dealing with nerve impingement and don’t know what to do first? The first step is understanding what causes it. This is key for getting better. Start by talking to health experts and looking at treatment options that suit your situation.
- Consult with healthcare professionals to diagnose the severity of nerve damage.
- Regular follow-ups to monitor nerve healing progress.
- Engage in recommended physical therapy exercises to aid recovery.
Addressing nerve impingement early can lower the risk of serious damage. It also makes treatment for trauma-induced back pain more effective.
Symptoms Signaling Sciatica
Knowing when sciatica starts is key to getting help early and avoiding long-lasting pain. This part talks about the main symptoms that mean someone might have sciatica. Spotting these signs early helps tell sciatica apart from other back or leg pains.
Radiating leg pain is a big sign of sciatica. This pain begins in the lower back, moves down through the buttocks, and goes along the back of the leg. It follows the path of the sciatic nerve indicators, making it a clear sign.
Another sign of sciatica is neurological symptoms. These include:
- Numbness in parts of the leg or foot
- A tingling feeling, like pins and needles
- Weakness in the leg, affecting foot movement
Having these symptoms, especially if they get worse, shows the need for a professional check. Symptoms like radiating leg pain and weakness can make everyday tasks hard. This includes walking, sitting for long times, or standing.
Knowing these signs helps people tell sciatica from less serious issues, like muscle sprains. If you have many symptoms of sciatica at once, see a doctor who knows about nerve problems. They can talk about your symptoms and how to possibly diagnose sciatica.
Seeing a doctor early when you notice these neurological symptoms and sciatic nerve indicators can really help. The right treatment can make life better. So, understanding sciatica signs not only helps with early spotting but also in dealing with this nerve issue more effectively.
Diagnosing Sciatica (Lumbar Radiculopathy)
It’s important to accurately diagnose sciatica to plan the best treatment. Doctors use patient history, exams, and diagnostic imaging to confirm sciatica and its causes.
A key tool is the lumbar MRI. It shows detailed pictures of the body’s inside. This helps find problems like disc herniation or spinal stenosis that press on the sciatic nerve.
The nerve conduction study is also vital in sciatica assessment. It checks how fast electrical signals move along nerves. This helps find where nerve damage is.
This mix of an MRI and a nerve conduction study gives a clear view of the sciatic nerve’s condition. It helps in creating focused treatment plans.
| Diagnostic Tool | Purpose | Benefit |
|---|---|---|
| Lumbar MRI | Visualize spinal structures | Detects anomalies like herniated discs |
| Nerve Conduction Study | Assess nerve functionality | Identifies exact location of nerve impairment |
Using these top-notch diagnostic tools confirms sciatica. It also guides in managing and planning treatment, making sure patients get care that fits their specific needs.
Treatment Options for Sciatica
Living with sciatica can make daily tasks tough. But there are many ways to find relief and heal. The sciatica treatment world is wide, with many choices based on your condition’s severity and cause. These include non-surgical methods and advanced surgical options. Let’s take a look at some treatments backed by science. They range from simple management to physical therapy, and surgery if needed.
Conservative Treatments
Before thinking about surgery, experts often suggest non-surgical treatments. This includes medication to lower inflammation and lessen pain. Chiropractic care is also vital. It can help align your spine, easing sciatic nerve pressure. Lifestyle changes, like better ergonomics and managing weight, also help. They improve your spine’s health and lower the chance of making your sciatica worse.
Physical Therapy
Physical therapy is a big part of treating sciatica without surgery. It uses methods to strengthen spinal support muscles, boost flexibility, and increase movement range. Custom exercise plans help soothe sciatic pain and stop it from coming back. Physical therapists might also use TENS or ultrasound to help manage sciatica symptoms.
Surgical Approaches
If non-surgical treatments don’t work, or if nerve compression is bad, surgery could be the next step. Surgery now aims to be less invasive. This helps patients recover faster and see better results. Procedures like microdiscectomy or laminectomy are done to ease sciatic nerve pressure, often reducing pain right away. Doctors note that surgery can be key for those with severe sciatica that hasn’t improved with other treatments.

