Over 32.5 million adults in the United States live with Osteoarthritis, also known as Degenerative Joint Disease. This makes it a leading cause of disability across the nation. Such a big number shows how joint degeneration affects our community’s health. Moreover, it highlights the need to understand this common condition. Osteoarthritis doesn’t only affect older people; it impacts individuals of all ages. It causes painful symptoms and limitations that disrupt lives.
The term Degenerative Joint Disease describes the slow breakdown of joint cartilage, which is better known as Osteoarthritis. Being the most common form of Arthritis, it comes with many symptoms and challenges. These challenges need to be addressed for maintaining good joint health. This article aims to offer a detailed look at Osteoarthritis. We will cover its symptoms, treatments, and strategies for effective management to help those in need.
Key Takeaways
- Osteoarthritis is a leading cause of disability affecting millions in the U.S.
- Understanding the disease is vital for managing symptoms and maintaining joint health.
- Degenerative Joint Disease can affect adults of all ages, not just the elderly.
- Symptom management and treatment options are essential for improving quality of life.
- Educational resources on Osteoarthritis can empower individuals to take an active role in their health care.
Introduction to Osteoarthritis
Osteoarthritis is the most common form of arthritis. It affects millions around the globe. This condition happens when cartilage, which cushions bones in joints, wears down over time. This leads to joint pain, stiffness, and less mobility.
Understanding osteoarthritis means knowing its main signs. These include joint pain, stiffness, swelling, and trouble moving. For people with this disease, osteoarthritis treatment focuses on easing symptoms and helping joints work better.
As we go further, we’ll look into osteoarthritis’s causes, symptoms, and treatments. We’ll also discuss how to live well with this disease. Each part will give important info on managing osteoarthritis and keeping a good quality of life.
The next sections will cover detailed information on:
- The causes of osteoarthritis
- How to spot symptoms and their development over time
- How osteoarthritis compares with other types of arthritis
- New and upcoming osteoarthritis treatment options
- Tips for handling everyday joint pain and stiffness
This intro helps us better understand osteoarthritis. It prepares those affected to manage their treatment and lifestyle changes better.
Exploring the Causes of Degenerative Joint Disease
It’s crucial to grasp the complex causes of degenerative joint disease. This understanding aids patients and healthcare providers in managing and preventing joint damage. Age, genetics, and lifestyle are key factors. They influence symptoms and cartilage wear in osteoarthritis.
The Role of Aging in Joint Health
Cartilage resilience decreases with age, affecting joint health. This loss of flexibility and moisture ups the risk of damage. As a result, people face increased osteoarthritis symptoms, complicating everyday life.
Genetic Factors Influencing Osteoarthritis
Genes play a big role in osteoarthritis risk. Some genetic markers specifically make cartilage wear down faster. This means the body struggles more to repair damaged cartilage, worsening osteoarthritis for those at risk.
Environmental and Lifestyle Impact
What we do and where we work matter for joint health. High-impact sports or repetitive jobs can speed up cartilage wear. Also, carrying extra weight puts more strain on joints like knees and hips, making osteoarthritis symptoms worse because of the added pressure.
Identifying the Symptoms of Osteoarthritis
Osteoarthritis symptoms can really get in the way of daily life. They can make moving around and doing everyday tasks hard. It’s important to spot these signs early to manage the condition well. Here’s a look at the common symptoms of osteoarthritis.
- Joint Pain: The most common symptom is joint pain. This pain often gets worse with activity but feels better with rest.
- Joint Stiffness: Stiffness in the affected joint is common. It’s especially noticeable in the morning or after being still for a while.
- Reduced Flexibility: Losing flexibility in the joint can be a big problem. It makes it difficult to do daily tasks.
- Swelling: Swollen joints are a sign too. This can come with tenderness and is caused by fluid buildup.
- A grating sensation: A rough, grating sound or feeling in the joint can occur. This is because the bones are rubbing together.
The severity of osteoarthritis symptoms can change. It depends on which joints are affected and how far along the condition is. The table below shows how symptoms generally appear at different stages of osteoarthritis:
| Stage of Osteoarthritis | Joint Pain | Joint Stiffness | Other Symptoms |
|---|---|---|---|
| Early Stage | Mild, occasional pain during movement | Morning stiffness, lasts less than 30 minutes | Slight swelling, possible soft clicking sounds |
| Moderate Stage | More consistent pain, aggravated by activity | Stiffness after inactivity or at end of day | Increased swelling, joint tenderness |
| Advanced Stage | Persistent and intense pain, even at rest | Significant stiffness, limited mobility | Large swelling, joint deformity, grating sensation |
The Anatomy of a Joint Affected by Osteoarthritis
Learning about joint anatomy helps us understand how Osteoarthritis causes joint degeneration. A normal joint has smooth cartilage at the bone ends. It also has a synovial membrane for making lubricating fluid. Plus, a sturdy joint capsule keeps the joint safe and stable.
Osteoarthritis brings many harmful changes to joints. The cartilage wears down, leading to cartilage degeneration. This loss means bones may touch each other. That can hurt and cause more harm.
The disease can also cause bone spurs, or osteophytes. These hard growths form at the edges of joints and can hurt and make movement stiff.
The synovial fluid’s ability to lubricate the joint can drop. This happens because of inflammation in the synovial membrane. The inflammation makes the pain and damage to the joint worse.
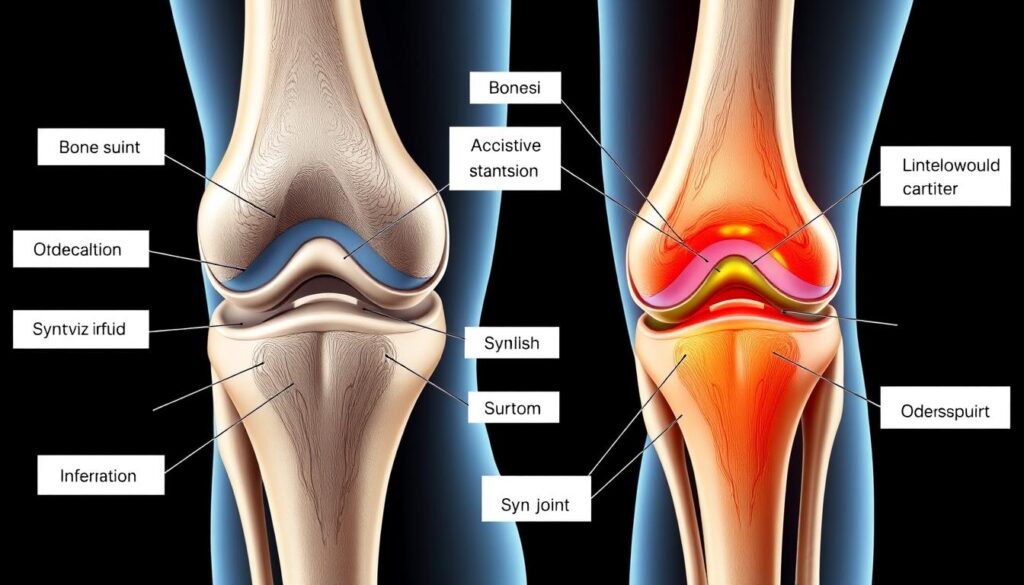
Osteoarthritis changes how a joint works. This leads to less movement and ongoing pain. Knowing these changes is vital for the right diagnosis and treatment.
Stages of Osteoarthritis Progression
Osteoarthritis develops through stages, each with more symptoms and joint problems. Knowing these stages helps manage the disease and plan treatments. It’s a condition where joints break down over time.
Early Stage Osteoarthritis
Early osteoarthritis starts with mild joint pain and stiffness. This usually happens after being still or when waking up. At this point, X-rays might show tiny bone spurs or a bit of joint space loss. The cartilage isn’t as strong and can’t cushion the bones well.
Advanced Degenerative Joint Disease
As osteoarthritis worsens, joint pain and stiffness get bad. The joints can’t move as freely. Some call it crippling. Cartilage may wear away totally in some spots. This can cause bone-on-bone rubbing, which is very painful and can make inflammation worse.
Osteoarthritis doesn’t just hurt the body; it can hit hard emotionally. When it’s hard to move, life’s quality can drop a lot.
Spotting these stages lets doctors and patients fight osteoarthritis together better. Each stage might need a different kind of care. Early on, changing your lifestyle or physiotherapy might help. Later, you might need drugs or even surgery.
Differentiating Between Osteoarthritis and Other Forms of Arthritis
Knowing the differences between Osteoarthritis and other arthritis types is key. Osteoarthritis happens when cartilage breaks down. This leads to joint pain and stiffness. Other kinds, like rheumatoid arthritis and psoriatic arthritis, are caused by the body attacking its own joints.
To make it clear, let’s compare them. This helps us understand joint health better. It also shows why different treatments are needed.
| Characteristic | Osteoarthritis | Rheumatoid Arthritis | Psoriatic Arthritis |
|---|---|---|---|
| Main symptoms | Joint pain, stiffness, limited range of motion | Swelling, pain, and redness in multiple joints | Joint pain, swelling, and stiffness, skin rashes |
| Typical joints affected | Knees, hips, fingers, and spine | Hands, wrists, knees, and feet | Hands, feet, neck, back, and knees |
| Onset of symptoms | Gradual | Sudden and symmetrical | Can be gradual or sudden, often with skin symptoms first |
| Treatment focus | Managing symptoms, improving joint function | Immune system suppression, reducing inflammation | Controlling inflammation, preventing joint damage |
Getting the right diagnosis is crucial for effective arthritis treatment. We differentiate Osteoarthritis from others by looking at symptoms and treatment. This ensures patients get the specific care they need for better joint health.
Diagnosing Osteoarthritis
Diagnosing osteoarthritis takes several steps. It involves looking at the patient’s history, a physical check-up, and medical images. Doctors like rheumatologists often work with primary care providers to spot this joint disease. Knowing the signs and how they change is key to spotting osteoarthritis early.
The first step in diagnosing osteoarthritis is talking about the patient’s symptoms and health background. A physical exam comes next. Here, the doctor checks for tenderness, swelling, and how well joints move. They use this info to figure out the best treatment plan based on where and how severe the symptoms are.
| Diagnostic Method | Description | Role in Diagnosing Osteoarthritis |
|---|---|---|
| Patient History | Review of symptoms and medical history | Identifies potential longevity and severity of condition |
| Physical Examination | Assessment of joint tenderness and movement | Observes physical manifestations of the disease |
| Imaging Tests | X-rays, MRI, and ultrasound | Visualizes joint degradation and cartilage loss |
| Lab Tests | Blood tests to rule out other conditions | Excludes other causes of joint pain |
Rheumatologists are key in diagnosing osteoarthritis, especially when it’s tricky. Symptoms might look like other types of arthritis. Tools like MRI and ultrasound give a closer look at the joints. This helps doctors make a precise diagnosis and craft a treatment just right for the patient.
The Impact of Osteoarthritis on Daily Living
Osteoarthritis is a common arthritis form that impacts many. It disrupts daily activities. It reduces the quality of life.
Challenges in Mobility and Routine Tasks
Osteoarthritis causes joint pain and stiffness. This leads to less mobility. Tasks like walking or opening jars get hard.
This condition makes doing everyday tasks tough. It can cause feelings of frustration. Sometimes, it even makes people need help from others.

Coping with Joint Pain and Stiffness
To live with osteoarthritis, people use different coping methods. These methods help manage pain and keep mobility.
- Engaging in regular, low-impact exercise to keep joints flexible and strengthen muscles around the joints.
- Using hot or cold treatments to ease joint stiffness and pain.
- Seeking physical therapy, which might include gentle stretching and strengthening exercises.
- Eating a well-balanced diet to maintain an optimal weight and reduce stress on joints.
- Utilizing assistive devices for tasks that are difficult to manage, such as grippers for opening jars or walking aids.
These strategies help with symptoms. They also improve life quality. They make daily tasks easier and increase independence.
Non-surgical Treatment Options for Osteoarthritis
Many ways exist to manage osteoarthritis without surgery. These non-surgical treatment options aim to better joint health and ease joint pain. From meds and physical therapy to changing your lifestyle, we’ll look at how these can help ease symptoms. And improve how well your joints work without needing surgery.
- Medications: OTC pain killers and anti-inflammatories are the go-tos. For worse pain, doctors might prescribe something stronger.
- Physical Therapy: Custom exercises help move better and strengthen muscles around joints. This is key in Osteoarthritis Treatment.
- Lifestyle Changes: Losing weight and eating better can lessen joint pressure and inflammation.
Physical therapy and staying active are great for joint pain and overall joint health. These steps can slow down osteoarthritis and help control symptoms. It’s also important to adjust everyday activities to lessen joint stress.
| Treatment Type | Benefits | Considerations |
|---|---|---|
| Medications | Pain relief, decreased inflammation | Watch out for side effects and how they mix with other meds |
| Physical Therapy | Better movement, more strength | Must stick with it regularly |
| Lifestyle Changes | Better weight control, overall health boost | Needs a long-lasting commitment |
These non-surgical methods are key in treating osteoarthritis fully. They help not just with easing symptoms but also in making life better for those dealing with this joint issue.
Innovations in Osteoarthritis Treatment
Doctors are working hard to meet the needs of people suffering from joint pain due to osteoarthritis. They are looking at new innovations in osteoarthritis treatment with hope. These new methods aim to improve life quality and might slow down the disease’s progress.

New drugs are being created to fight osteoarthritis more effectively. They do more than just ease symptoms. They try to stop the damage to joints from worsening. On top of that, breakthroughs in biotech are bringing us new treatments. Among these are gene therapy and biologic drugs, which fight the inflammation that causes osteoarthritis.
Alongside drug developments, regenerative medicine is making big strides in treating osteoarthritis. Treatments like stem cell therapy and PRP injections are becoming more popular. They could help fix damaged joint tissues. Researchers are studying these treatments to see how well they work and if they can give long-term relief and improve joint function.
- Biological therapies utilizing growth factors and cytokines to modulate joint inflammation and repair.
- Advanced imaging techniques that allow for earlier detection and personalized treatment planning.
- Integration of artificial intelligence to tailor treatments based on individual patient data and predictive modeling.
The field of osteoarthritis treatment is always moving forward, giving new hope. There are many studies underway that aim to find better ways to manage the disease. Thanks to this hard work, the future seems promising for people facing osteoarthritis.
Understanding Cartilage Degeneration in Osteoarthritis
Osteoarthritis involves the breaking down of joint structures, with cartilage degeneration being key. This breakdown is central to the condition’s symptoms, affecting joint health and how well it works.
Cartilage is the smooth material at the ends of bones in joints. It helps with movement and absorbs impacts. Yet, over time, wear and tear and biological factors cause this tissue to degrade. This loss involves collagen and proteoglycans, which keep cartilage strong and hydrated.
Knowing how cartilage breaks down helps us find better ways to deal with osteoarthritis progression. Looking into healing treatments and protective measures is crucial. Our goal is to slow down the damage and boost joint function. This improves life quality for those with the condition.
| Factor | Impact on Cartilage Degeneration | Potential Protective Strategy |
|---|---|---|
| Mechanical Stress | Accelerates wear and tear | Weight management, joint-friendly exercise |
| Biological Changes | Alters cartilage composition | Pharmacological interventions |
| Genetic Predisposition | Increases susceptibility | Early diagnosis and targeted therapy |
Improving joint health means more than just reducing cartilage loss. It also involves addressing things that make osteoarthritis progression worse. By adding lifestyle changes and new medical treatments, we can better manage symptoms and enhance how joints function in those with osteoarthritis.
Lifestyle Changes and Home Remedies for Joint Health
Managing osteoarthritis includes lifestyle changes and home remedies. These steps boost joint health, improve daily life, and enhance overall well-being. We will look into the benefits of exercise, physical therapy, and the right diet.
Exercise and Physical Therapy
Regular exercise and physical therapy are key for good joint health. They help by strengthening muscles around your joints, easing their load. Customized physical therapy increases flexibility, motion range, and reduces pain. Low-impact activities like swimming, cycling, and light aerobics are great choices.
Nutrition and Supplements
Your diet affects your joint health. Eating anti-inflammatory foods like omega-3 rich fish, green veggies, and nuts helps fight osteoarthritis inflammation. Also, supplements like glucosamine and chondroitin might improve your joints. But, always check with your doctor before starting supplements.
| Benefit | Exercise | Nutrition and Supplements |
|---|---|---|
| Reduces Joint Pain | Strengthens surrounding muscles, lessening pressure on joints | Anti-inflammatory foods reduce swelling |
| Improves Flexibility | Range of motion exercises enhance joint mobility | Essential nutrients aid in joint lubrication |
| Enhances Overall Health | Increases blood flow and aids in weight management | Optimal nutrition boosts immune response and overall well-being |
Making effective home remedies and lifestyle adjustments part of your osteoarthritis care can really help your joints. These actions reduce pain and symptoms, leading to a healthier and more active life.

When to Consider Surgery for Osteoarthritis
Finding the right time for joint surgery is key for those with severe joint disease. If pain and mobility don’t get better with medicine and changing your lifestyle, surgery might be an option. Not all osteoarthritis cases need surgery. Yet, if your daily life is really hard because of it, surgery might be needed.
Osteoarthritis treatment often ends up at surgery if the pain is bad, moving becomes hard, and life’s quality drops. Here are signs that surgery might be your next step:
- Persistent joint pain that does not improve with non-surgical treatments
- Joint stiffness that limits the ability to perform routine tasks
- Significant joint damage as depicted through imaging tests
- Loss of cartilage leading to bone rubbing against bone
Surgical choices can be less invasive like arthroscopy or more complex like joint replacement or osteotomy. Let’s look at these surgeries:
| Surgical Option | Description | Recovery Period | Suitability |
|---|---|---|---|
| Arthroscopy | Minimally invasive, involves inserting a camera to repair tissues | 4 to 6 weeks | Mild to moderate cases |
| Joint Replacement | Removal and replacement of the damaged joint with a prosthesis | 3 to 6 months | Severe cases with joint deformity |
| Osteotomy | Bone cutting to realign the joint and reduce pain | 2 to 3 months | Younger patients with limited arthritis |
Each surgery has its risks and benefits. The decision heavily leans on your specific health and lifestyle. Joint surgery is chosen when the good it can do is much more than the risks.
Conclusion
We’ve delved deep into Osteoarthritis, exploring this complex joint condition. We understand its causes, symptoms, and how it progresses. Knowing this helps in effectively handling joint pain.
It’s vital to know how osteoarthritis differs from other arthritis types. This knowledge leads to better treatment and living strategies.
There are many treatments for Osteoarthritis, from simple approaches to advanced surgeries. These treatments aim to improve life quality and function. It’s key to combine new medical breakthroughs with care tailored to each patient.
For anyone facing joint pain, creating a custom plan with doctors is key. This approach ensures the best management of Osteoarthritis.
The fight against Osteoarthritis isn’t over. Continuous research is shaping the future of how we treat it. Meanwhile, learning resources help patients play a part in their care.
Staying educated and working with doctors is essential for those with this joint disease. Together, managing Osteoarthritis becomes a united effort. It allows patients to enjoy life, despite chronic joint issues.

