
Introduction to Molluscum Contagiosum
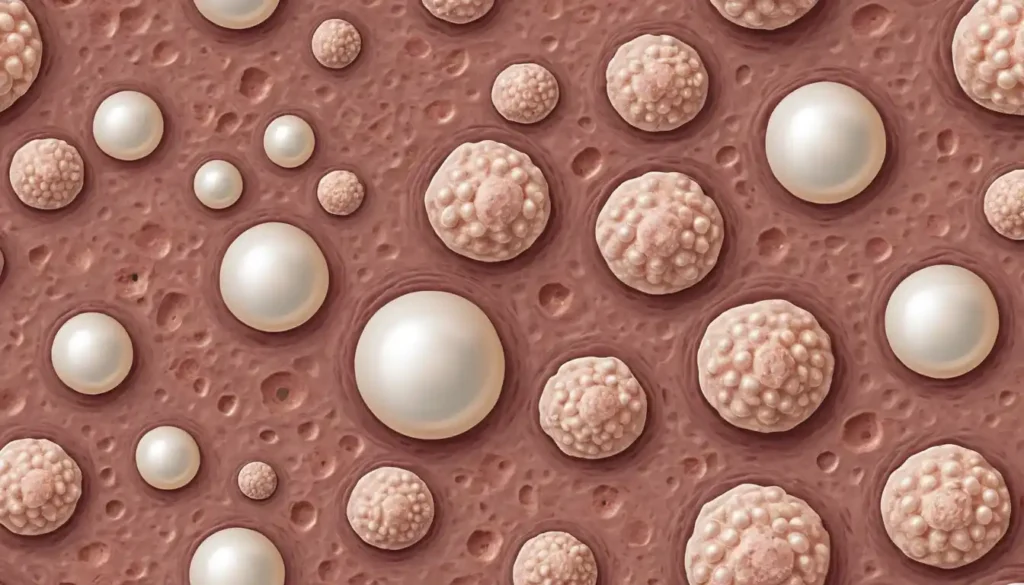
Molluscum contagiosum is a common viral skin infection that primarily affects children, but can also occur in adults. It is characterized by small, raised, pearl-like bumps on the skin.
Although generally harmless, these lesions can be bothersome due to their appearance and potential for spreading. This article explores the nature, causes, symptoms, and various treatment options for molluscum contagiosum.
What is Molluscum Contagiosum?
Understanding the Viral Nature of Molluscum Contagiosum
Molluscum contagiosum is caused by the molluscum contagiosum virus (MCV), a member of the poxvirus family. The infection results in distinctive skin lesions that are typically painless but may cause cosmetic concerns.
The virus resides within these bumps and can spread through direct contact or contact with contaminated objects.
Causes of Molluscum Contagiosum
Molluscum Contagiosum Virus (MCV): The Root Cause
The molluscum contagiosum virus is the sole cause of this condition. It spreads easily through skin-to-skin contact, making it prevalent among children who often engage in close physical activities.
How Molluscum Contagiosum Spreads
- Direct Contact: Touching the lesions of an infected person can transmit the virus.
- Contaminated Objects: Sharing towels, clothing, or toys with someone who has molluscum can lead to infection.
- Sexual Contact: In adults, the virus can be transmitted through sexual activity.
Risk Factors for Contracting Molluscum Contagiosum
- Children between ages 1 to 10: Most commonly affected due to frequent close contact and shared items.
- Weakened Immune System: Individuals with conditions such as HIV or those undergoing cancer treatments are more susceptible.
- Atopic Dermatitis: Skin conditions that compromise the barrier function increase risk.
Symptoms of Molluscum Contagiosum
Identifying the Characteristic Skin Bumps
The primary symptom of molluscum contagiosum is small, round bumps on the skin that are typically flesh-colored or pink. These bumps often have a dimpled center and vary in size from a pinhead to a pencil eraser.
Common Areas of the Body Affected by Molluscum Contagiosum
- Children: Lesions commonly appear on the face, trunk, arms, and legs.
- Adults: In cases of sexual transmission, bumps may appear on the genitals, lower abdomen, and inner thighs.
How to Differentiate Molluscum Contagiosum from Other Skin Conditions
Molluscum contagiosum lesions are distinct due to their central dimple and smooth texture. Unlike acne or warts, they are usually not inflamed unless irritated by scratching or rubbing.
How Molluscum Contagiosum is Diagnosed
Physical Examination for Molluscum Contagiosum
Diagnosis is typically made through a visual examination by a healthcare provider. The unique appearance of the lesions often allows for straightforward identification without additional testing.
Dermatoscopy and Other Diagnostic Tools
In some cases, dermatoscopy might be used to examine the lesions more closely. A skin biopsy may be conducted if there is uncertainty about the diagnosis or if other conditions need to be ruled out.
When to Seek Professional Diagnosis
Consult a healthcare provider if you suspect molluscum contagiosum, particularly if lesions persist or spread significantly. Professional evaluation ensures accurate diagnosis and appropriate management strategies.
When to Treat Molluscum Contagiosum
Understanding When Treatment is Necessary
Treatment for molluscum contagiosum is not always required, as the condition is generally self-limiting. However, treatment may be considered in the following scenarios:
- Cosmetic Concerns: If the lesions are in visible areas and cause embarrassment or self-consciousness.
- Discomfort: When bumps become itchy, irritated, or infected.
- Spread Prevention: To prevent transmission to others, especially in communal settings like schools or gyms.
Can Molluscum Contagiosum Go Away on Its Own?
Yes, molluscum contagiosum often resolves on its own without treatment within 6 to 12 months. However, in some cases, it may persist longer, up to several years.
Factors That Influence the Decision to Treat
- Age of the Patient: Children may not require treatment unless lesions are bothersome.
- Location and Number of Lesions: Extensive or facial lesions may warrant intervention.
- Immune Status: Immunocompromised individuals might need more aggressive treatment due to prolonged infection.
Topical Treatments for Molluscum Contagiosum
Over-the-Counter Creams and Lotions
Several OTC products can help manage molluscum contagiosum:
- Benzoyl Peroxide: Reduces bacterial load and inflammation around lesions.
- Salicylic Acid: Helps exfoliate the skin and promote lesion clearance.
Prescription Creams: Imiquimod, Tretinoin, and Cantharidin
- Imiquimod: An immune response modifier that helps clear lesions by boosting local immune activity.
- Tretinoin: A retinoid that promotes skin cell turnover and can help reduce lesion size.
- Cantharidin: Applied by a healthcare provider; causes blistering that helps remove lesions.
Salicylic Acid for Molluscum Contagiosum
Salicylic acid is a common treatment option due to its keratolytic properties, which help dissolve keratin plugs and clear lesions over time.
Invasive Treatments for Molluscum Contagiosum
Cryotherapy: Freezing the Lesions
Cryotherapy involves applying liquid nitrogen to freeze and destroy molluscum contagiosum lesions. This method is quick but may require multiple sessions for complete clearance.
Curettage: Scraping Off Bumps
Curettage involves using a small instrument to scrape off the lesions. It is effective but can be uncomfortable and may leave small scars.
Laser Therapy: Precise Removal of Molluscum Lesions
Laser therapy targets molluscum lesions with concentrated light beams, effectively removing them with minimal damage to surrounding tissue.
Electrocautery: Using Heat to Treat Molluscum Contagiosum
Electrocautery uses heat generated by electric current to burn off lesions. It is typically used for stubborn cases that do not respond to other treatments.
Home Remedies and Natural Treatments for Molluscum Contagiosum
Tea Tree Oil: A Popular Natural Option
Tea tree oil, known for its antiviral and antibacterial properties, can be used to treat molluscum contagiosum. However, it should be diluted with a carrier oil to avoid skin irritation.
Apple Cider Vinegar for Skin Lesions
Apple cider vinegar has been suggested as a natural remedy due to its acidity, which may help break down the keratin plugs in molluscum lesions. However, its effectiveness is not well-documented.
Coconut Oil and Other Soothing Remedies
Coconut oil, rich in fatty acids, can help soothe and moisturize the skin, potentially reducing inflammation around molluscum lesions. Other natural oils like olive oil and jojoba oil may also provide similar benefits.
Boosting the Immune System to Fight Molluscum Contagiosum
The Role of Immune System in Clearing the Virus
The immune system plays a crucial role in clearing molluscum contagiosum. A strong immune response can help eliminate the virus and prevent recurrence.
Foods and Supplements to Boost Immunity
- Vitamin C: Foods rich in vitamin C, such as citrus fruits and leafy greens, can help boost the immune system.
- Zinc: Zinc supplements or zinc-rich foods like oysters and beef can support immune function.
- Probiotics: Maintaining a healthy gut microbiome with probiotics can enhance overall immunity.
How Stress Management Can Improve Recovery
Stress can weaken the immune system, making it harder for the body to fight off molluscum contagiosum. Engaging in stress-reducing activities like meditation, yoga, or deep breathing exercises can help manage stress and support recovery.

Treatment Options for Children with Molluscum Contagiosum
Safe Treatments for Pediatric Patients
For children, treatment options are often focused on gentle, non-invasive methods to avoid discomfort and potential scarring. Topical treatments like salicylic acid or imiquimod may be recommended.
How to Prevent Molluscum from Spreading Among Children
- Good Hygiene: Encourage children to wash their hands frequently and avoid touching the lesions.
- Avoid Sharing Personal Items: Prevent sharing of towels, clothing, and toys to reduce transmission risk.
- Covering Lesions: Use bandages or clothing to cover lesions in public areas like schools and daycare centers.
Managing Molluscum Contagiosum in Schools and Daycare
Educational settings should emphasize hygiene practices and provide guidance on managing outbreaks to prevent widespread transmission.
Molluscum Contagiosum Treatments for Adults
Adult-Specific Treatment Approaches
Adults may require more aggressive treatment due to the potential for longer duration of infection and higher risk of transmission. Invasive treatments like cryotherapy or curettage may be considered.
Addressing Molluscum in Immunocompromised Individuals
Immunocompromised adults may need specialized treatment plans that address their weakened immune status. This may include antiviral medications or other targeted therapies.
Treating Molluscum Contagiosum in Sensitive Areas
For adults with molluscum contagiosum in sensitive areas, such as the genitals, treatment options may be limited to avoid discomfort and potential complications. Topical treatments are often preferred in these cases.
Alternative Therapies for Molluscum Contagiosum
Light Therapy and Photodynamic Treatments
Light therapy, including photodynamic therapy (PDT), uses specific wavelengths of light to target and destroy molluscum contagiosum lesions. This method can be effective for those who do not respond to traditional treatments, though it may require multiple sessions.
Immune Modulating Treatments for Resistant Cases
For cases that are resistant to standard therapies, immune modulating treatments can be considered. These treatments aim to enhance the body’s immune response to clear the virus more effectively. Options may include topical immunomodulators like imiquimod or oral medications that boost immune function.
Clinical Trials and New Experimental Approaches
Ongoing clinical trials are exploring new treatment options for molluscum contagiosum, including novel topical agents and systemic therapies. Participation in a clinical trial may provide access to cutting-edge treatments not yet widely available.
Complications and When to See a Doctor
Secondary Infections: When Molluscum Becomes Infected
Secondary bacterial infections can occur if molluscum lesions are scratched or irritated. Signs of infection include increased redness, swelling, pain, or pus. If these symptoms develop, it is important to seek medical attention for appropriate treatment.
Scarring and Skin Discoloration: Potential Side Effects of Treatment
Some treatments for molluscum contagiosum, particularly invasive ones like curettage or electrocautery, may lead to scarring or skin discoloration. Discuss potential side effects with a healthcare provider before proceeding with treatment.
How to Prevent Further Skin Damage
- Avoid Picking or Scratching: This can lead to infection and scarring.
- Use Gentle Skincare Products: Opt for mild cleansers and moisturizers to minimize irritation.
- Follow Post-Treatment Care Instructions: Adhere to any aftercare guidelines provided by your healthcare provider.
Preventing the Spread of Molluscum Contagiosum
Hygienic Practices to Prevent Transmission
- Regular Hand Washing: Wash hands frequently with soap and water.
- Avoid Sharing Personal Items: Do not share towels, clothing, or personal care items with others.
- Clean Surfaces: Regularly disinfect surfaces that may come into contact with the virus.
Avoiding Skin Contact in Public Areas (Gyms, Pools, etc.)
- Use Protective Barriers: Wear flip-flops in communal showers and avoid direct contact with shared gym equipment.
- Cover Lesions: Use bandages or clothing to cover lesions when in public settings.
Managing Outbreaks in Family Settings
- Educate Family Members: Ensure everyone understands how the virus spreads and the importance of hygiene.
- Isolate Affected Individuals: Minimize contact between infected individuals and others until lesions resolve.
Lifestyle and Daily Care During Molluscum Contagiosum Treatment
Skincare Routine for Affected Areas
Maintaining a gentle skincare routine is crucial during treatment:
- Cleanse Gently: Use a mild, fragrance-free cleanser to wash affected areas daily.
- Moisturize: Apply a soothing, non-comedogenic moisturizer to keep the skin hydrated and reduce irritation.
- Avoid Harsh Products: Steer clear of products containing alcohol or strong fragrances that could irritate the skin.
Avoiding Irritants and Triggers for Flare-Ups
- Fragrance-Free Products: Opt for hypoallergenic skincare products to minimize irritation.
- Loose Clothing: Wear loose-fitting clothes to prevent friction against lesions.
- Avoid Hot Showers: Use lukewarm water to prevent drying out the skin.
Wearing Protective Clothing to Minimize Spread
Covering lesions with clothing or bandages can help prevent the spread of molluscum contagiosum, especially in communal settings or when engaging in physical activities.
How Long Does Molluscum Contagiosum Treatment Take?
Recovery Timeline for Different Treatment Methods
The duration of treatment varies depending on the method used:
- Topical Treatments: May take several weeks to months for full resolution.
- Invasive Treatments (e.g., Cryotherapy, Curettage): Often result in quicker lesion removal, but multiple sessions may be needed.
- Natural Remedies: Typically require consistent application over a longer period to see results.
Factors That Affect Healing Time
- Immune System Strength: A robust immune system can expedite recovery.
- Extent of Infection: Larger or more widespread infections may take longer to resolve.
- Adherence to Treatment: Consistent application of treatments as directed enhances effectiveness.
When to Expect Full Resolution of Symptoms
Most cases of molluscum contagiosum resolve within 6 to 12 months, but some may persist longer. Regular follow-ups with a healthcare provider can help monitor progress and adjust treatment as needed.

Molluscum Contagiosum Treatment Costs
Comparing the Cost of Treatments: OTC vs. Prescription
- Over-the-Counter (OTC) Options: Generally more affordable, but may require longer use for effectiveness.
- Prescription Treatments: Often more expensive due to higher potency and specialized formulations.
Insurance Coverage for Molluscum Treatments
Insurance coverage varies; some plans may cover prescription treatments or procedures like cryotherapy, while others may not. It’s advisable to check with your insurance provider for specific coverage details.
Affordable Home Remedies and Low-Cost Alternatives
Natural remedies such as tea tree oil or apple cider vinegar offer low-cost alternatives, though their effectiveness may vary. Always consult with a healthcare provider before starting any new treatment.
Post-Treatment Care for Molluscum Contagiosum
Preventing Recurrence After Treatment
- Maintain Good Hygiene: Continue regular hand washing and avoid sharing personal items.
- Boost Immunity: Support your immune system through a balanced diet and healthy lifestyle choices.
Dealing with Post-Inflammatory Hyperpigmentation
Hyperpigmentation can occur after lesions heal. Use gentle exfoliants and brightening agents like vitamin C serums to help even out skin tone over time.
Scarring Prevention Tips After Treatment
To minimize scarring:
- Avoid picking or scratching at healing lesions.
- Use silicone gel sheets or scar creams as recommended by a dermatologist.
Frequently Asked Questions about Molluscum Contagiosum
Can Molluscum Contagiosum Spread Through Towels?
Yes, molluscum contagiosum can spread through sharing towels, clothing, or other personal items that have come into contact with the virus.
Is Molluscum Contagiosum a Sexually Transmitted Infection?
Molluscum contagiosum is not exclusively a sexually transmitted infection (STI), but it can be transmitted through sexual contact. The virus can spread through skin-to-skin contact, making it a concern in sexual health.
Can You Treat Molluscum Contagiosum at Home?
While some home remedies may help manage symptoms, it is generally recommended to consult a healthcare provider for proper diagnosis and treatment. This ensures effective management and minimizes the risk of complications.
How Long Does It Take for Molluscum Contagiosum to Clear?
The time it takes for molluscum contagiosum to clear varies depending on the treatment method and individual immune response. Most cases resolve within 6 to 12 months, but some may persist longer.
Are There Permanent Treatments for Molluscum Contagiosum?
There are no permanent treatments that guarantee the virus will not recur. However, effective management strategies can help prevent future outbreaks.
Conclusion
Managing and Treating Molluscum Contagiosum Effectively
Managing molluscum contagiosum requires a comprehensive approach that includes proper diagnosis, appropriate treatment, and preventive measures to avoid spreading the virus.
The Importance of Patience and Consistency in Treatment
Treatment for molluscum contagiosum can be lengthy and requires patience and consistency. Adhering to treatment plans and maintaining good hygiene practices are crucial for effective management.
Long-Term Outlook for Those Affected by Molluscum Contagiosum
While molluscum contagiosum can be bothersome, it is generally not a serious condition. With proper management and preventive measures, individuals can reduce the risk of future outbreaks and maintain healthy skin. This concludes the comprehensive guide on molluscum contagiosum. If you have any further questions or need additional information, feel free to ask!
Final Thoughts
Molluscum contagiosum is a common skin condition that can be effectively managed with the right approach. By understanding its causes, symptoms, and treatment options, individuals can take proactive steps to prevent its spread and maintain healthy skin. Remember, patience and consistency are key in managing this condition. Stay informed, stay healthy

