Hair loss is a universal concern that affects millions of people worldwide, transcending age, gender, and cultural boundaries. For many, the onset of hair loss can be a distressing experience, impacting self-esteem and overall well-being. Androgenetic Alopecia, commonly referred to as male or female pattern baldness, is the most common form of hair loss, driven by a complex interplay of genetics, hormones, and environmental factors.
According to research, Androgenetic Alopecia affects up to 50% of both men and women, with the condition manifesting differently across genders. In men, it often presents as a receding hairline and balding at the crown, while women typically experience diffuse thinning at the top of the scalp.
Key Takeaways
- Hair loss is a widespread issue affecting both men and women globally.
- Androgenetic Alopecia is the most common form of hair loss.
- The condition is influenced by genetics, hormones, and environmental factors.
- Symptoms and presentation differ between men and women.
- Understanding the causes and treatment options is crucial for managing the condition.
Understanding Androgenetic Alopecia
Androgenetic alopecia, commonly known as male or female pattern baldness, is a widespread condition affecting millions worldwide. It is characterized by a gradual thinning of hair, particularly on the scalp, due to the influence of androgens.
Definition and Prevalence
Androgenetic alopecia is a hereditary condition that leads to hair loss. It affects both men and women, though the pattern and severity can vary between genders. The prevalence increases with age, impacting a significant portion of the population over 50. In this condition, hair follicles become sensitive to dihydrotestosterone (DHT), a potent derivative of testosterone, leading to a gradual shrinkage of the follicles and a shortening of the hair growth cycle.
The condition is not just a cosmetic issue; it can have psychological effects, impacting self-esteem and confidence. Understanding its causes and mechanisms is crucial for developing effective treatments.
The Hair Growth Cycle
The hair growth cycle consists of four distinct phases: anagen, catagen, telogen, and exogen. The anagen phase is the active growth phase, lasting from 2 to 6 years. During this time, hairs grow actively. The catagen phase is a short transitional period lasting about 1 to 2 weeks, followed by the telogen phase, which is a resting phase that lasts about 3 to 5 months.
In androgenetic alopecia, the anagen phase shortens, and the percentage of hairs in the telogen phase increases. This disruption leads to a reduction in hair density and an overall decrease in growth rate, resulting in thinner, shorter hairs.
Causes of Pattern Hair Loss
Pattern hair loss, a condition affecting millions, is driven by a complex interplay of genetic and hormonal factors. Understanding these underlying causes is essential for developing effective treatment strategies.
Genetic Factors
Genetic predisposition plays a significant role in pattern hair loss. Individuals with a family history of baldness are more likely to experience hair loss. Research has shown that multiple genetic variants contribute to the susceptibility to androgenetic alopecia. The condition is considered polygenic, meaning it is influenced by several different genes.
The inheritance pattern is complex, involving both maternal and paternal genes. Studies have identified several genetic loci associated with an increased risk of developing androgenetic alopecia. These genetic factors influence the sensitivity of hair follicles to androgens, leading to hair loss.
Hormonal Influences
Hormonal influences, particularly androgens, are critical in the development of pattern hair loss. Dihydrotestosterone (DHT), a potent metabolite of testosterone, is the primary hormonal driver of hair loss in men. DHT affects DHT-sensitive hair follicles in the scalp, leading to hair thinning and eventual loss.
The enzyme 5-alpha reductase converts testosterone to DHT, and elevated levels of this enzyme have been documented in the scalp of individuals with pattern hair loss. In men, pattern hair loss typically begins after puberty, when androgen levels significantly increase.
The role of hormones in female pattern hair loss is more complex. While androgens are also implicated, female pattern hair loss can occur in women with normal androgen levels. The role of estrogen remains unclear, though the increased prevalence of hair loss after menopause suggests hormonal shifts play a significant role.
| Hormone | Role in Hair Loss | Effect on Men | Effect on Women |
|---|---|---|---|
| Dihydrotestosterone (DHT) | Primary driver of hair loss | Significant hair loss | Contributes to hair loss |
| Testosterone | Precursor to DHT | Increased levels post-puberty | Normal levels, but can be converted to DHT |
| Estrogen | Role unclear, potential protective effect | Not directly implicated | May influence hair loss post-menopause |
Male Pattern Baldness
The onset of male pattern baldness can occur shortly after puberty, with its progression influenced by a combination of genetic and hormonal factors. This condition is characterized by a distinct pattern of hair loss, typically starting with a receding hairline and thinning at the crown.
Characteristic Patterns and Progression
Male pattern baldness follows a predictable pattern, often beginning with hair loss around the temples and crown. As it progresses, the hairline recedes, and the area of baldness expands, potentially leading to complete baldness.
The progression of male pattern baldness can be influenced by various factors, including genetics, hormonal imbalances, and environmental factors such as stress and poor nutrition.
| Stage | Description |
|---|---|
| I | Minimal hair loss, primarily around the temples |
| II | Noticeable hair recession around the temples, forming an ‘M’ shape |
| III | Significant hair loss at the crown, with possible bridging between the receding hairline and the crown |
The Norwood Scale
The Norwood Scale is a classification system used to measure the extent of male pattern baldness. It ranges from Stage I (minimal hair loss) to Stage VII (complete baldness at the top of the head).
This scale helps in understanding the progression and severity of the condition, aiding in the selection of appropriate treatments.
Age of Onset and Risk Factors
Male pattern baldness can begin as early as the late teenage years. Approximately 25% of men show signs by age 21, and this number increases to 50% by age 50.
- Early onset (before age 30) often indicates a stronger genetic predisposition.
- Supplemental testosterone or anabolic steroid use can accelerate hair loss.
- Environmental factors like smoking, poor nutrition, and chronic stress may exacerbate the condition.
Understanding these risk factors can help in managing and potentially slowing down the progression of male pattern baldness.
Female Pattern Hair Loss
Hair loss in women, particularly female pattern hair loss, is a complex issue that requires a nuanced understanding of its causes and manifestations. Unlike male pattern baldness, female pattern hair loss presents with distinct characteristics and is influenced by a variety of factors including genetics, hormones, and age.
Distinctive Features and Patterns
Female pattern hair loss is characterized by a diffuse thinning of hair across the scalp, particularly on the top and crown, rather than the distinct baldness seen in men. This condition can lead to a reduction in hair density but typically does not result in complete baldness. The hair loss is often more pronounced after menopause, suggesting a hormonal influence.
Hormonal factors play a significant role in female pattern hair loss. Conditions such as polycystic ovarian syndrome (PCOS) can accelerate hair loss in younger women due to hormonal imbalances. Moreover, the transition through different life stages such as pregnancy, postpartum, and menopause can also affect hair loss due to changes in estrogen and androgen levels.
The Ludwig Scale
The Ludwig Scale is used to classify the severity of female pattern hair loss. It categorizes hair loss into three stages, from mild thinning to more pronounced balding. Understanding the stage of hair loss is crucial for determining the most appropriate treatment plan.
- The scale helps in assessing the extent of hair loss.
- It provides a standardized way to communicate the severity of the condition.
- Treatment options can be tailored based on the stage of hair loss.
Hormonal Considerations in Women
Hormonal imbalances are a critical factor in female pattern hair loss. An imbalance of estrogen and androgens can lead to hair loss. Additionally, conditions like thyroid disorders and iron deficiency can exacerbate or mimic female pattern hair loss, making a comprehensive blood panel essential in the diagnostic workup.
In conclusion, female pattern hair loss is a multifactorial condition that requires a comprehensive approach to diagnosis and treatment. Understanding the distinctive features, using classification scales like the Ludwig Scale, and considering hormonal influences are crucial steps in managing this condition effectively.
Symptoms of Androgenetic Alopecia
Androgenetic alopecia, commonly known as male or female pattern baldness, manifests through distinct symptoms that vary between individuals. Understanding these symptoms is crucial for early detection and treatment.
Early Warning Signs
The initial signs of androgenetic alopecia include a gradual thinning of hair, particularly on the scalp. This condition is characterized by the conversion of terminal hairs into vellus hairs in areas sensitive to DHT, as illustrated in Norwood and Ludwig pattern diagrams. Hair loss is typically painless; however, if accompanied by pain, irritation, or redness, it may indicate a different type of hair loss.
Progression of Hair Thinning
As androgenetic alopecia progresses, the affected areas expand, and the degree of thinning intensifies. In men, this typically follows the Norwood scale, with recession at the temples joining with thinning at the crown. Women experience a widening area of diffuse thinning on the crown. The progression is generally slow but can accelerate due to hormonal changes, stress, or illness.
| Characteristics | Men | Women |
|---|---|---|
| Pattern of Hair Loss | Recession at temples, thinning at crown | Diffuse thinning on crown |
| Progression Rate | Variable, can be rapid | Generally slow, can accelerate |
| Scalp Condition | Remains healthy | Remains healthy |
The scalp remains healthy throughout the progression, distinguishing pattern hair loss from inflammatory or scarring forms of alopecia.
Diagnosing Pattern Hair Loss

Diagnosing androgenetic alopecia, commonly known as pattern hair loss, involves a combination of clinical evaluation and, in some cases, additional testing. This comprehensive approach helps healthcare professionals accurately determine the underlying causes of hair loss and develop an effective treatment plan.
Clinical Examination Methods
A thorough clinical examination is the first step in diagnosing pattern hair loss. This involves assessing the scalp and hair to identify characteristic patterns of hair loss. Healthcare professionals examine the extent and distribution of hair thinning, particularly in the vertex and frontal areas of the scalp.
- Visual inspection to assess the pattern and extent of hair loss
- Pull test to evaluate the ease with which hairs are pulled out
- Examination of the scalp for signs of inflammation or scarring
Laboratory Testing
In some cases, laboratory tests may be necessary to rule out other causes of hair loss or to confirm the diagnosis. These tests can include:
- Blood tests to check for hormonal imbalances or deficiencies
- Tests to rule out autoimmune or infectious causes of hair loss
Scalp Biopsy
A scalp biopsy is rarely necessary for diagnosing typical cases of pattern hair loss but can be valuable when the clinical presentation is atypical or when coexisting scalp conditions are suspected. The procedure involves taking two 4-mm punch biopsies in the direction of hair growth, allowing for both horizontal and vertical sectioning.
Histologic features of male and female pattern hair loss include terminal hair miniaturization, increased percentage of telogen hairs, and a decreased ratio of terminal to vellus or vellus-like hairs. The biopsy can also help rule out inflammatory or scarring alopecias that may coexist with or mimic pattern hair loss.
Differential Diagnosis
When diagnosing hair loss, it’s essential to consider various conditions that may mimic androgenetic alopecia. A thorough differential diagnosis helps in accurately identifying the underlying cause of hair loss.
Telogen Effluvium
Telogen effluvium is a condition characterized by excessive hair shedding, often triggered by stress, hormonal changes, or nutritional deficiencies. It typically presents with diffuse hair loss across the scalp, rather than the patterned loss seen in androgenetic alopecia.
Alopecia Areata
Alopecia areata is an autoimmune condition that causes patchy hair loss. It can be distinguished from androgenetic alopecia by its unpredictable pattern of loss and the presence of smooth, round bald patches on the scalp.
Other Hair Loss Conditions
Other forms of alopecia that may present similarly to male and female pattern hair loss include traction alopecia, trichotillomania, central centrifugal cicatricial alopecia, lichen planopilaris, and frontal fibrosing alopecia. These conditions can be identified by their distinct characteristics, such as the location and pattern of hair loss, presence of inflammation, and scalp damage.
| Condition | Characteristics |
|---|---|
| Traction Alopecia | Caused by chronic tension on hair follicles, often due to tight hairstyles, affecting the hairline. |
| Trichotillomania | A compulsive hair-pulling disorder, creating irregular patches of broken hair. |
| Central Centrifugal Cicatricial Alopecia | Inflammation starting at the crown, spreading outward, causing permanent loss and scarring. |
Medical Treatments for Androgenetic Alopecia
For those suffering from androgenetic alopecia, several medical treatment options are available, each with its benefits and considerations. The choice of treatment often depends on the extent of hair loss, patient preference, and the presence of any underlying health conditions.
FDA-Approved Medications
The FDA has approved two primary medications for the treatment of androgenetic alopecia: minoxidil and finasteride. Minoxidil, available in topical form, is applied directly to the scalp to stimulate hair growth and slow down hair loss. It is suitable for both men and women.
Finasteride, on the other hand, is an oral medication primarily prescribed for men. It works by inhibiting the production of dihydrotestosterone (DHT), a hormone involved in the development of androgenetic alopecia. While effective, finasteride may have side effects, and its use in women, especially those who are pregnant or planning to become pregnant, is generally not recommended due to potential risks.
Off-Label Treatment Options
Besides FDA-approved medications, several treatments are used off-label for androgenetic alopecia. Dutasteride, a more potent 5-alpha-reductase inhibitor than finasteride, has been used for men with more resistant cases, showing greater efficacy in reducing DHT levels. For women, spironolactone, an androgen receptor blocker, is often prescribed, particularly for those showing signs of androgen excess.
Other off-label treatments include low-dose oral minoxidil, which has gained popularity for its potential to offer greater efficacy than topical application, albeit with a higher risk of systemic side effects. Ketoconazole shampoo is another option, believed to have mild anti-androgenic properties. Various combination therapies are also explored to enhance treatment outcomes.
Topical Treatments

The quest for effective hair loss solutions has led to the development of various topical treatments that aim to promote hair growth and halt balding progression. These treatments are applied directly to the scalp, targeting the root cause of hair loss.
Minoxidil and Its Mechanism
Minoxidil is a well-known topical treatment for hair loss, particularly for androgenetic alopecia. It works by widening the hair follicle, prolonging the anagen phase, and thus promoting hair growth. The exact mechanism is not fully understood, but it’s believed to enhance blood flow to the scalp, nourishing the hair follicles.
The application of minoxidil is straightforward, typically involving a twice-daily application to the affected areas of the scalp. Results can vary, with some users experiencing significant hair growth while others may see a slowing in hair loss.
Other Topical Solutions
Beyond minoxidil, several other topical treatments show promise for pattern hair loss. These include:
- Topical finasteride, which may provide local DHT inhibition with reduced systemic absorption.
- Topical anti-androgens like fluridil and alfatradiol, available in some countries, work by blocking DHT at the follicular level.
- Ketoconazole shampoo (1-2%) has mild anti-androgenic properties and may enhance the efficacy of other treatments.
- Peptide-based formulations, such as copper peptides, and growth factor solutions derived from plant or biotechnology sources.
These treatments offer various mechanisms of action and can be used alone or in combination with other therapies to address hair loss effectively.
Oral Medications
Oral medications have emerged as a crucial component in the treatment arsenal against androgenetic alopecia, offering hope to those experiencing hair loss. These medications can be particularly effective in halting or slowing down the progression of pattern baldness.
Finasteride for Men
Finasteride is a well-established oral medication for treating male pattern baldness. It works by inhibiting the conversion of testosterone to dihydrotestosterone (DHT), a hormone involved in hair loss. Studies have shown that finasteride can significantly slow down hair loss and, in some cases, promote hair regrowth.
Key Benefits: Effective in slowing down hair loss, promotes hair regrowth in some cases.
Treatment Options for Women
For women, treatment options are more nuanced due to the potential risks associated with certain medications. Spironolactone is commonly prescribed off-label as an anti-androgen therapy. Topical minoxidil remains the only FDA-approved medication for female pattern hair loss.
Treatment Considerations: Spironolactone blocks testosterone binding to hair follicle receptors. For postmenopausal women, finasteride or dutasteride may be considered due to the eliminated risk of birth defects.
Combination therapies, including oral anti-androgens and topical minoxidil, are often more effective than monotherapy, offering a comprehensive approach to managing female pattern hair loss.
Surgical and Advanced Treatments
For individuals experiencing significant hair loss due to androgenetic alopecia, surgical and advanced treatments offer a viable solution. These treatments are designed to restore hair growth and improve the appearance of balding areas.
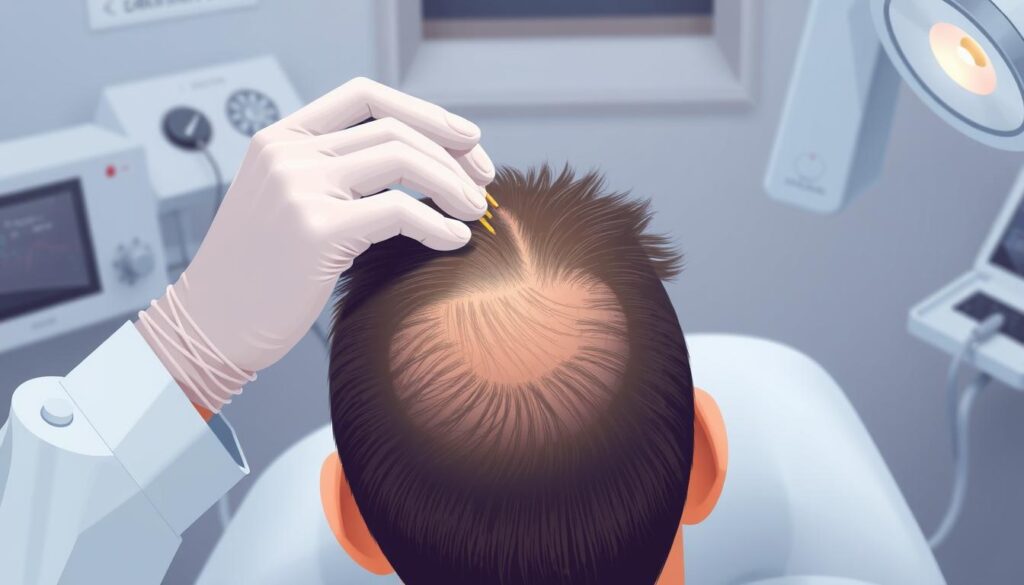
Hair Transplantation Techniques
Hair transplantation is a surgical procedure that involves relocating hair follicles from one part of the scalp to another. This technique has evolved over the years, with methods such as follicular unit transplantation (FUT) and follicular unit extraction (FUE) being widely used. These procedures aim to achieve natural-looking hair growth in areas affected by balding.
The success of hair transplantation depends on various factors, including the skill of the surgeon, the quality of the donor hair, and the patient’s overall health. As a result, it’s essential to consult with a qualified professional to determine the best course of treatment.
Emerging Therapies
In addition to surgical options, several emerging therapies are being explored for their potential in treating hair loss. These include platelet-rich plasma (PRP) therapy, which involves injecting concentrated platelets into the scalp to stimulate hair follicle activity. Other treatments, such as low-level laser therapy (LLLT) and exosome therapy, are also being investigated for their efficacy in promoting hair growth.
These innovative approaches offer new hope for individuals experiencing hair loss. While some of these therapies are still in the experimental stages, they represent a promising area of research and potential future treatments for androgenetic alopecia.
Psychological Impact of Hair Loss

Experiencing hair loss can be distressing, with far-reaching psychological implications for those affected. The emotional toll of androgenetic alopecia can be significant, particularly for women, who may feel a loss of femininity and youth.
Mental Health Considerations
The psychological impact of hair loss can be substantial, leading to feelings of shame and isolation. Women, in particular, may feel that they are alone in their experience, exacerbating the emotional distress. It’s essential to acknowledge that hair loss is a common condition affecting many individuals.
Mental health support is crucial in addressing the emotional aspects of hair loss. Seeking help from mental health professionals can provide individuals with coping strategies and techniques to manage their condition.
Coping Strategies
Effective coping strategies can help individuals manage the psychological impact of hair loss. Some approaches include:
- Seeking support from mental health professionals who can provide cognitive-behavioral techniques.
- Joining support groups, either online or in-person, to connect with others experiencing similar challenges.
- Utilizing cosmetic approaches such as hairstyling techniques, hair fibers, and scalp micropigmentation to manage appearance concerns.
- Practicing stress management techniques to mitigate the negative cycle of stress and hair loss.
- Educating oneself about the condition and available treatments to regain a sense of control.
By adopting these strategies, individuals can better cope with the psychological impact of hair loss and improve their overall well-being.
Conclusion
In conclusion, androgenetic alopecia is a prevalent condition that necessitates a holistic approach to management, incorporating medical, surgical, and psychological support. Pattern hair loss is a progressive condition that affects both men and women, albeit with different patterns and severity.
Early diagnosis and intervention are crucial in managing hair loss. Treatments are most effective when initiated before significant hair loss occurs, helping to maintain existing hair and potentially stimulate regrowth. A comprehensive treatment plan often yields the best results, combining FDA-approved medications, off-label treatments, and surgical interventions when necessary.
The psychological impact of hair loss should not be underestimated. Addressing these aspects is an essential part of comprehensive care. While pattern hair loss cannot be completely cured with current treatments, ongoing research into its pathophysiology continues to drive the development of new therapies that may offer improved outcomes.
Patients should work closely with healthcare providers specializing in hair disorders to develop individualized treatment plans. With proper treatment and realistic expectations, most individuals with androgenetic alopecia can achieve meaningful improvements in hair density and appearance, positively impacting their quality of life over time.
By understanding the causes of hair loss, including genetic and hormonal factors, and addressing the condition comprehensively, individuals can effectively manage pattern hair loss and mitigate its impact on their body and well-being.

