A startling fact has emerged in healthcare: over 7,000 individuals across 27 states have been affected by a new type of health threat. This pathogen is a drug-resistant yeast that poses a serious challenge to modern medicine.
The illness primarily impacts vulnerable people in hospitals or long-term care facilities. Those with weakened immune systems or medical devices in their bodies are at highest risk. Healthy individuals with robust immune systems usually do not get sick, but they can still carry and transmit the infection to others.
What makes this pathogen so concerning is its resistance to multiple antifungal medications. This characteristic makes it exceptionally difficult to treat once an infection occurs. Public health authorities are paying close attention due to its rapid spread.
Understanding this threat is the first step toward protection. Awareness and proper infection prevention and control measures are critical for combating its spread in healthcare settings and protecting public health.
Key Takeaways
- A drug-resistant yeast has infected thousands of people across more than half of U.S. states.
- This health threat primarily affects individuals in healthcare settings with other medical conditions.
- The pathogen is resistant to multiple antifungal drugs, making treatment difficult.
- Healthy people can carry and spread the infection without getting sick themselves.
- Public health authorities consider this an urgent threat requiring immediate attention.
- Prevention through strict infection control is the most effective defense strategy.
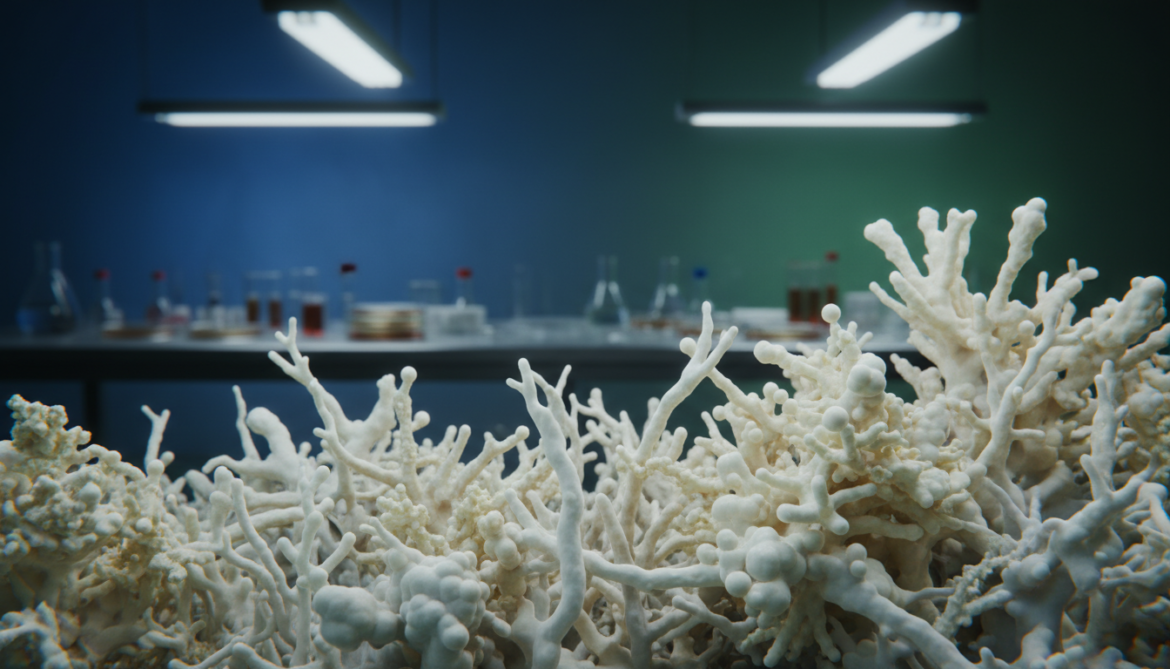
Overview of Candida Auris Emergence in the United States
In 2016, U.S. health authorities identified a new multidrug-resistant pathogen that would challenge existing infection control protocols. This marked the beginning of coordinated surveillance efforts across healthcare facilities nationwide.
Background on the Drug-Resistant Fungal Infection
The pathogen demonstrates resistance to all major antifungal medications. This characteristic makes treatment exceptionally difficult for affected patients.
Clinical cases represent confirmed infections from diagnostic specimens. These indicate active disease rather than simple colonization.
Recent Trends and Case Statistics
Current data shows concerning growth patterns. The Centers for Disease Control and Prevention reports rapid spread across multiple states.
More than half of U.S. states reported clinical cases in 2025. Tennessee confirmed 189 infections that year alone.
| State | Reported Cases (2025) | Healthcare Facilities Affected |
|---|---|---|
| Tennessee | 189 | Multiple hospitals |
| California | 157 | Long-term care centers |
| Florida | 142 | Acute care facilities |
| New York | 135 | Nursing homes |
The global spread includes 61 countries across six continents. This demonstrates the international scope of this health challenge.
Superbug Fungus Candida Auris: A Growing Challenge in Healthcare Settings

Medical institutions worldwide confront a persistent adversary that thrives in clinical environments designed for healing. This pathogen demonstrates remarkable resilience in healthcare settings where vulnerable patients receive treatment.
Spread and Survival in Hospitals and Nursing Homes
The organism spreads efficiently through contaminated medical equipment and surfaces. Shared devices like catheters and breathing tubes become transmission vehicles in hospitals.
Environmental persistence makes containment difficult. The pathogen survives on bed railings, equipment, and other surfaces for extended periods.
| Transmission Route | Common Locations | Prevention Challenge |
|---|---|---|
| Contaminated surfaces | Bed railings, furniture | Complete disinfection difficulty |
| Medical equipment | Catheters, ventilators | Equipment sharing necessity |
| Person-to-person contact | Patient rooms, common areas | Asymptomatic carrier transmission |
Epidemiologist Melissa Nolan explains the challenge: “It’s really good at just being, generally speaking, in the environment. So if you have it on a patient’s bed for example, on the railing, and you go to wipe everything down, if in whatever way maybe a couple of pathogens didn’t get cleared, then they’re becoming resistant.”
Biological mechanisms enhance its survival. Proteins in the cell wall enable strong adhesion to human skin and surface colonization.
This deadly fungus forms protective layers that block drug penetration. Combined with environmental resistance, this creates significant containment challenges in nursing homes and hospitals.
Identifying Risks and Symptoms of Candida Auris Infections
Healthcare providers face significant challenges in identifying this multidrug-resistant pathogen. The clinical signs often resemble other common healthcare-associated infections.
Recognizing Clinical Signs and Warning Symptoms
Symptoms of auris infections can be subtle and nonspecific. Fever and chills that don’t improve with antibiotics may indicate fungal involvement.
Bloodstream infections typically cause sepsis-like symptoms. The pathogen is notoriously difficult to detect using standard laboratory methods.
Diagnostic delays can prove fatal for vulnerable individuals. Early identification requires specialized testing not available in all facilities.
Understanding Patient Vulnerability and Underlying Conditions
Certain medical conditions dramatically increase infection risk. Patients with weakened immune systems face the greatest danger.
Those requiring invasive devices have significantly higher susceptibility. Medical equipment provides direct entry points into the body.
| Risk Factor | Affected Population | Prevention Priority |
|---|---|---|
| Weakened immune system | Cancer patients, transplant recipients | High |
| Invasive medical devices | Patients with catheters or ventilators | Critical |
| Prolonged hospitalization | Long-term care residents | Medium-high |
| Recent surgery | Post-operative patients | Medium |
Epidemiologist Melissa Nolan emphasizes the treatment challenge: “If you get infected with this pathogen that’s resistant to any treatment, there’s no treatment we can give you to help combat it. You’re all on your own.”
Mortality rates range from 30% to 60% for invasive cases. This underscores the critical need for early detection in care settings.
Prevention, Treatment, and Control Measures

Effective containment requires a multi-layered approach combining prevention, surveillance, and treatment innovations. Healthcare systems must implement comprehensive strategies to protect vulnerable individuals.
Best Practices for Infection Control in Healthcare Facilities
Robust protocols form the foundation of protection. Environmental cleaning, patient screening, and facility communication are essential components.
State health departments coordinate with hospitals to enhance practices. They implement early detection systems and rapid reporting for new cases.
| Prevention Measure | Implementation Level | Key Benefit |
|---|---|---|
| Enhanced environmental cleaning | All healthcare facilities | Reduces surface transmission |
| Patient screening protocols | High-risk units | Early case identification |
| Inter-facility communication | Regional networks | Prevents cross-transmission |
| Staff education programs | All care settings | Improves adherence to guidelines |
Advances in Antifungal Drugs and Future Research
Current treatment faces significant challenges. Resistance mechanisms limit drug effectiveness against certain pathogens.
CDC epidemiologist Dr. Meghan Lyman emphasizes the urgency: “The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control.”
Research focuses on novel agents with broad-spectrum activity. Scientists study immune-based modalities for high-risk patients.
Future directions include improved diagnostic tests and global monitoring systems. These advances will enhance our ability to manage difficult infections.
Conclusion
Public health authorities continue to monitor dangerous microorganisms that resist conventional treatments. Candida auris represents a significant challenge with thousands of documented cases this year.
This pathogen poses the greatest danger to individuals with weakened immune systems or underlying health conditions. Those requiring medical devices face particularly high risk.
The combination of drug resistance and environmental persistence makes auris infections difficult to manage. Medical teams encounter challenges in both diagnosis and treatment.
Some patients face mortality rates between 30% and 60%, highlighting the serious nature of this disease. Vigilant infection control remains essential for protecting vulnerable people in healthcare settings.
Ongoing research offers hope through new treatments and diagnostic technologies. Coordinated efforts among healthcare providers, families, and public health officials can reduce transmission over time.
While the threat is serious, continued surveillance and prevention practices help safeguard public health. These measures work to control the spread of this resilient pathogen.