One in five colorectal cancers in the United States is diagnosed after the disease has already spread, according to the Centers for Disease Control and Prevention. That late timing often traces back to missed signals. This section highlights the early signs of colon cancer you shouldn’t ignore.
Experts at Mayo Clinic and the American Cancer Society report seven recurring colon cancer symptoms. These include persistent changes in bowel habits, rectal bleeding or blood in the stool, abdominal pain or cramping, ongoing gas or bloating, fatigue and weakness, unexplained weight loss, and the sensation of incomplete evacuation. Many people have no symptoms early, which makes attention to subtle colon cancer warning signs even more important.
Women may misread lingering cramps, bloating, or altered stools as irritable bowel syndrome, endometriosis, menstruation, or menopause. When these signs of colon cancer last beyond two weeks, clinicians advise prompt testing. That may include stool tests, bloodwork, and a colonoscopy.
Screening can prevent disease. A colonoscopy can find and remove precancerous polyps before they turn into cancer. Noticing early signs of colon cancer and acting quickly can change the outcome.
Key Takeaways
- Seven key colon cancer symptoms: bowel habit changes, blood in stool, abdominal pain, gas/bloating, fatigue, weight loss, and incomplete evacuation.
- Many cases show no symptoms early, so subtle colon cancer warning signs matter.
- If symptoms persist for two weeks or more, seek evaluation with stool tests, bloodwork, and colonoscopy.
- Women may misattribute symptoms to IBS, endometriosis, menstruation, or menopause.
- Early detection saves lives; colonoscopy can remove precancerous polyps.
- Know the early signs of colon cancer and act quickly if anything feels off.
Understanding Colon Cancer
Colon cancer starts quietly. It grows in the colon, the long, first segment of the large intestine. Many cases begin as small polyps that seem harmless at first. Over years, some polyps can turn into cancer. Because early changes rarely cause clear symptoms of colorectal cancer, screening plays a central role in a timely colon cancer diagnosis.
What Is Colon Cancer?
Colon cancer is a disease of DNA damage and unchecked cell growth. The cells form tumors that can invade nearby tissue and, in time, spread to distant organs. Colorectal cancer is the combined term for cancers of the colon and the rectum.
Most polyps do not cause pain or bleeding. That is why colonoscopy matters. This test uses a flexible tube with a camera to view the entire colon. It can find and remove polyps or take a biopsy in the same visit, helping confirm a colon cancer diagnosis while reducing future risk.
Risk Factors for Colon Cancer
Risk rises with age, especially after 50, though rates are increasing under 50. In the United States, Black adults face a higher incidence and mortality. Personal history also matters, including prior colorectal cancer or polyps, and long-standing inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease. Inherited syndromes, such as Lynch syndrome and familial adenomatous polyposis, elevate risk at younger ages.
- Family history of colon or rectal cancer in first-degree relatives
- Low-fiber, high-fat eating patterns and frequent red or processed meat
- Physical inactivity, obesity, and diabetes with insulin resistance
- Smoking, heavy alcohol use, and prior abdominal radiation
Some risks are more often noted in women, including family histories that feature ovarian cancer, prior breast or endometrial cancer, and long-term hormone therapy. Type 2 diabetes, metabolic syndrome, and sedentary routines with low fiber can add to the burden. Pregnancy-related changes, such as gestational diabetes, and chronic pelvic conditions may blur the typical symptoms of colorectal cancer, delaying evaluation and colon cancer diagnosis.
Common Symptoms of Colon Cancer
Recognizing colon cancer symptoms early can make a real difference. The early signs of colon cancer often start subtly, then become more persistent. If any of the issues below continue despite diet changes or over-the-counter remedies, it’s time to speak with a healthcare professional.
Changes in Bowel Habits
Shifts in routine bathroom patterns are among the most reported early signs of colon cancer. Watch for diarrhea, constipation, or narrowed stools that last more than a few days.
A feeling that the bowel doesn’t empty fully after a movement is another red flag. A new, ongoing struggle to pass stool without a clear cause may indicate a blockage from a growth.
- Duration matters: symptoms that persist for weeks deserve evaluation.
- Pattern changes: sudden, unexplained shifts in frequency or stool shape are concerning.
Blood in Stool
Bleeding can appear in different ways. Bright red streaks may signal lower intestinal bleeding, while dark maroon or black, tarry stools can suggest bleeding higher up.
Sometimes the bleeding is microscopic and not visible. This can lead to iron-deficiency anemia found on routine blood tests. Because hemorrhoids and menstruation can mask warning signs, tests like FIT or FOBT and a colonoscopy are often advised to clarify the source.
- Look for color changes that persist or recur.
- Combine symptom tracking with medical testing when in doubt.
Unexplained Weight Loss
Rapid, unintentional weight loss ranks among notable colon cancer symptoms. It reflects the body’s response to inflammation and the tumor’s metabolic demands.
Losing 5–10% of body weight over a few months without trying is one of the early signs of colon cancer that warrants a thorough workup. Appetite changes and reduced nutrient absorption can add to the drop on the scale.
- Track weight weekly to spot trends early.
- Pair weight changes with other symptoms to inform the next steps.
Digestive Issues Related to Colon Cancer
Digestive changes can be early signals that the gut is under strain. Paying attention to subtle shifts helps you spot potential signs of colon cancer and understand how symptoms of colorectal cancer can show up day to day.
Abdominal Pain and Cramping
Ongoing belly pain that keeps returning or lingers is a common red flag. It may feel sharp, crampy, or like a deep ache that settles on one side. Unlike routine indigestion, it often does not ease with antacids or simple diet changes.
Some people notice a growing sense of pressure or fullness. Discomfort can flare after bowel movements or even wake you at night. These patterns belong on your radar as possible signs of colon cancer and should be viewed within the broader symptoms of colorectal cancer you may be tracking.
- Pain that persists for weeks
- Cramping tied to changes in stool
- Localized tenderness that returns
Persistent Gas or Bloating
Gas and bloating that do not match your meals or cycle—and resist usual fixes—deserve attention. When the bowel narrows, gas can build and linger. This may signal slowed transit or a partial blockage.
If bloating teams up with constipation, nausea, or vomiting, the concern for obstruction rises. Keep notes on frequency, timing, and triggers. A clear record helps you and your clinician weigh these signs of colon cancer alongside other symptoms of colorectal cancer for a fuller picture.
- Bloating that worsens over time
- Minimal relief after passing gas
- New tightness or swelling in the abdomen
Additional Symptoms to Note
Some colon cancer warning signs appear subtle at first. When they persist or grow worse, they can hint at issues beyond routine stomach bugs or stress. Paying attention to energy levels and stomach upset can offer useful clues and can also shape colon cancer prognosis.
Why this matters: Systemic symptoms point to whole-body strain, while obstructive symptoms point to blocked bowel flow. Both patterns can guide a quicker path to care and may influence colon cancer prognosis.
Fatigue and Weakness
Long-lasting fatigue is one of the overlooked colon cancer warning signs. Slow internal bleeding from a tumor can cause iron-deficiency anemia. That may lead to weakness, pale skin, lightheadedness, shortness of breath, and poor exercise tolerance.
Routine blood work sometimes flags low red blood cell counts before other symptoms show up. For women, ongoing tiredness without another clear cause should prompt a check for hidden gastrointestinal blood loss. Early evaluation supports a more informed colon cancer prognosis.
- Persistent fatigue that sleep does not fix
- Breathlessness during normal walks
- Dizziness when standing up fast
Nausea and Vomiting
Nausea and vomiting can arise when a growing mass narrows the bowel. This is more likely with tumors in the ascending or transverse colon. The pattern often includes cramping, bloating, and reduced appetite, adding to key colon cancer warning signs.
Vomiting with constipation and a swollen abdomen may signal a late-stage blockage and needs urgent care. While many common bugs cause nausea, cancer-related symptoms tend to progress and resist over-the-counter remedies. Recognizing this pattern can inform timing of care and may affect colon cancer prognosis.
- Waves of nausea that worsen week to week
- Vomiting plus abdominal distension
- Little relief from standard OTC treatments
Early Detection Strategies
Most early colon changes are silent. That makes timely colon cancer screening a practical way to find trouble before symptoms start and to guide a clear colon cancer diagnosis when signs appear.
Think of screening as routine maintenance for your colon. Polyps can be located and removed long before they turn dangerous, helping you stay ahead of disease.
Importance of Regular Screenings
Experts such as Mayo Clinic advise most adults at average risk to begin at about age 45. If you have a family history, hereditary syndromes, or inflammatory bowel disease, talk with your clinician about starting earlier.
Early findings allow simpler care. Localized disease often has far better outcomes, so staying on a schedule matters whether you feel fine or not.
For anyone under 50 with symptoms—like rectal bleeding or iron-deficiency anemia—do not wait. Prompt testing supports faster colon cancer diagnosis and safer decisions.
Recommended Tests for Colon Cancer
- Colonoscopy: The gold standard. It views the entire colon, removes polyps, and supports biopsy of suspicious areas during the same visit.
- Stool-based tests: FOBT and FIT look for hidden blood. They are noninvasive and useful between colonoscopies, with positive results leading to follow-up.
- CT colonography: A detailed imaging option when a traditional scope is not possible or is incomplete.
- Other tools: MRI or capsule endoscopy may be considered when anatomy is complex. A physical exam and blood tests for anemia often start the workup.
Use a plan that fits your risk and preferences. A steady approach to colon cancer screening supports accurate colon cancer diagnosis and helps catch problems when they are easiest to treat.
Lifestyle Factors Impacting Symptoms
Daily habits can shape how the gut feels and functions. Food choices, movement, alcohol, and tobacco all interact with the digestive tract. Smart changes may ease discomfort, highlight the early signs of colon cancer, and work alongside colon cancer screening for a clearer health picture.
Diet and Nutrition Considerations
A low-fiber, high-fat Western pattern is linked with higher colorectal risk in several studies. Emphasize fiber-rich foods like oats, berries, beans, and whole-grain bread. They add bulk, support regularity, and may reduce irritation that can mask the early signs of colon cancer.
Lean proteins and plant-forward meals help replace frequent red or processed meats. Aim for a colorful plate loaded with fruits, vegetables, and whole grains. Limit alcohol and avoid tobacco; these steps align with guidance from the Mayo Clinic and support safer digestion between colon cancer screening intervals.
- Quick swaps: choose brown rice over white; snack on nuts instead of chips.
- Hydration: drink water with meals to help fiber do its job.
- Moderation: keep alcohol to low levels and pair it with food.
Exercise and Physical Activity
Regular movement supports gut motility and weight control. Start with 30 minutes most days—brisk walking, cycling, or swimming. If you are inactive, build up slowly and track consistency like a training plan.
Physical activity can lower inflammation and stabilize blood sugar, which matters for those with obesity or diabetes. A steady routine may reduce confusing GI flare-ups and make the early signs of colon cancer easier to notice, while staying on track with colon cancer screening keeps detection timely.
- Easy wins: take stairs, park farther away, stretch after sitting.
- Mix it up: combine cardio with light strength training twice a week.
- Stay accountable: use a smartwatch or app to nudge daily goals.
When to Consult a Healthcare Professional
If something feels off, trust your instincts. Timely care can turn uncertainty into a clear plan, and early assessment speeds the path to answers. Knowing the colon cancer warning signs—and what to bring to an appointment—helps you advocate for yourself.
Your body often whispers before it shouts. Track what you notice, how long it lasts, and what makes it better or worse. This record supports a more accurate colon cancer diagnosis if your clinician suspects it.
Recognizing Warning Signs
Seek medical advice if symptoms persist beyond two weeks. Many causes are benign, yet evaluation is key to find the source and treat it early.
- Ongoing changes in bowel habits, including constipation, diarrhea, or narrowing of stools.
- Visible or suspected blood in stool, dark tarry stools, or a metallic smell.
- Sensation of incomplete evacuation after a bowel movement.
- Unexplained fatigue or weakness that may signal anemia.
- Abdominal pain or cramping that does not resolve.
- Persistent bloating or gas without a clear trigger.
- Unintentional weight loss over weeks or months.
Women under 50 should push for evaluation if symptoms linger. Mislabeling issues as IBS, stress, or hormone shifts can delay a colon cancer diagnosis.
Preparing for Your Doctor Visit
Bring specifics. Clear details help your clinician connect symptoms to possible causes and decide on next steps for testing.
- Log duration, frequency, and progression of symptoms. Note stool color, consistency, and any narrowing.
- Record associated pain, timing, and triggers such as meals, fiber, or medications.
- Document family history of colorectal, ovarian, endometrial, or breast cancer, plus any prior polyps or IBD.
- List medications and supplements, including iron, NSAIDs, or anticoagulants.
- Be ready for initial tests: a complete blood count for anemia, stool tests like FIT or FOBT, and imaging or colonoscopy if indicated.
Ask what each test looks for and when results will return. Understanding the plan reduces stress and keeps the focus on the colon cancer warning signs most relevant to your case.
If appointments are hard to schedule, request triage for persistent symptoms. A thorough workup supports a timely colon cancer diagnosis and appropriate follow-up.
The Role of Family History
Family history can shape your personal risk in clear ways. When close relatives have had colon or rectal cancer, the odds climb. That is why understanding the symptoms of colorectal cancer and planning timely colon cancer screening work hand in hand for prevention.
Importance of Genetic Factors
Inherited syndromes such as Lynch syndrome and familial adenomatous polyposis change the timeline. These conditions can lead to earlier onset and subtle warning signs. Some families also see patterns that include rectal or ovarian cancers.
If multiple first-degree relatives were diagnosed, or if one relative was diagnosed at a young age, the signal grows stronger. In these settings, even mild symptoms of colorectal cancer deserve prompt attention.
- Lynch syndrome: higher lifetime risk, often earlier in adulthood.
- Familial adenomatous polyposis: numerous polyps with rapid progression if untreated.
- Clusters of related cancers across generations may indicate a shared genetic driver.
Screening Guidelines for Those with Family History
For people at increased risk, experts at Mayo Clinic recommend earlier and more frequent colon cancer screening. Colonoscopy is preferred because it can find and remove precancerous polyps and collect biopsies during the same visit.
Timing varies by risk. Some high-risk pathways begin before age 45, with shorter intervals between exams. Discuss the plan with a healthcare team to match your family pattern, personal history, and any symptoms of colorectal cancer that arise.
- Start screening earlier based on the youngest age at diagnosis in a close relative.
- Use colonoscopy as the primary test to detect and treat lesions in one session.
- Repeat at shorter intervals if polyps are found or risk remains high.
Proactive surveillance aligns with evidence-based care. When you pair vigilant tracking of symptoms of colorectal cancer with tailored colon cancer screening, you strengthen your odds of catching changes when they are most manageable.
How Symptoms May Vary by Stage
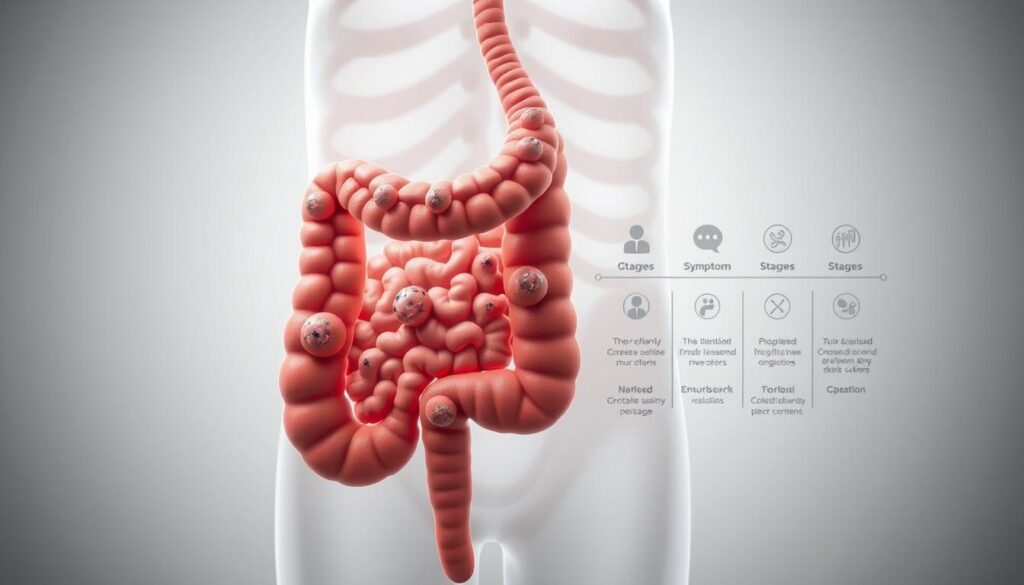
Stage matters because the body sends different signals as disease progresses. Knowing the early and late patterns helps you track the signs of colon cancer and discuss colon cancer prognosis with your care team. Small clues often appear first, then build into clearer warnings.
Early Stage Symptoms
Many early tumors stay quiet. When symptoms show up, they tend to be subtle and easy to miss. Watch for mild shifts in bowel habits that persist despite diet tweaks.
- Off-and-on cramping or gentle bloating after meals
- Tiny amounts of blood you cannot see, leading to iron‑deficiency anemia on lab tests
- Stools that look normal most days, but changes recur over weeks
If gentle remedies fail to help, that pattern can be one of the signs of colon cancer that deserves attention. Early detection can improve colon cancer prognosis by allowing treatment before spread.
Advanced Stage Indicators
As tumors grow, blockage risks rise. Discomfort often shifts from occasional to steady and intense, and daily routines become harder to manage.
- Marked constipation or pencil‑thin stools
- Severe cramping with nausea and vomiting from obstruction
- Pronounced fatigue, weakness, and ongoing weight loss
- Findings that suggest spread: enlarged liver on exam, yellowing of the skin or eyes, or shortness of breath
These later changes represent clear signs of colon cancer that warrant urgent evaluation. At this point, the colon cancer prognosis depends on extent of spread, overall health, and how quickly care begins.
Colon Cancer Treatment Options
Care teams now match therapy to stage, tumor biology, and your goals. This tailored plan improves comfort and can strengthen colon cancer prognosis. Decisions draw on guidance from the National Comprehensive Cancer Network and the National Cancer Institute, paired with your preferences.
Screening can change the path. A colonoscopy may remove precancerous polyps before they turn dangerous. When cancer is found early and is resectable, outcomes are often strong, which supports a more favorable colon cancer prognosis.
Surgical Interventions
Surgery is the mainstay for localized disease. Surgeons remove the tumor and nearby lymph nodes to stage the cancer and reduce the chance of return. Many patients go home faster thanks to minimally invasive methods like laparoscopy and enhanced recovery protocols.
What to expect:
- Local excision or polypectomy when cancer is confined to a polyp or superficial layer.
- Segmental colectomy with lymph node dissection for most resectable tumors.
- Restoration of bowel continuity whenever possible; temporary ostomy in select cases.
Clear margins and adequate node sampling guide next steps. These details help refine colon cancer treatment options and shape the colon cancer prognosis shared during follow-up visits.
Chemotherapy and Radiation
Chemotherapy may be used after surgery to lower relapse risk or as first-line care for spread to other organs. Regimens can include fluoropyrimidines with oxaliplatin or irinotecan. Targeted drugs and immunotherapy are considered when molecular testing shows a good fit.
Key points to discuss with your oncologist:
- Molecular markers such as MSI status, RAS, BRAF, and HER2 that inform drug choice.
- Treatment goals—cure, control, or symptom relief—shaping timing and intensity.
- Supportive care for side effects, including nausea control, neuropathy prevention, and fatigue management.
Radiation is used more often for rectal tumors but can help relieve pain or bleeding in select colon cases. When integrated with systemic therapy, these colon cancer treatment options can maintain quality of life and may improve colon cancer prognosis in specific settings.
Coping with Diagnosis and Treatment
Facing a colon cancer diagnosis can feel overwhelming. Clear information, steady support, and a plan for colon cancer treatment options can reduce fear and help you make choices that fit your life. Small steps—one call, one question—build control.
Emotional Support Resources
Trusted guidance matters when decisions arrive fast. Resources from Mayo Clinic, the American Cancer Society, the National Comprehensive Cancer Network, and the National Cancer Institute explain colon cancer treatment options in plain language and outline what to expect after a colon cancer diagnosis.
Palliative care guidance from NCCN focuses on comfort, symptom relief, and quality of life at any stage. This support can work alongside active treatment, helping with pain, nutrition, sleep, and stress.
- Ask for a nurse navigator to coordinate appointments and testing.
- Request social work support for insurance, work leave, and transportation.
- Use patient guidelines to prepare questions for your oncology visit.
Centers recognized for gastrointestinal care—such as Mayo Clinic, noted by U.S. News & World Report—often provide integrated services, including nutrition counseling, mental health care, and survivorship planning.
Connecting with Colon Cancer Groups
Peer communities offer real-world tips and solidarity. Advocacy groups help you track symptoms, compare colon cancer treatment options, and speak up during visits after a colon cancer diagnosis.
- Join moderated forums or local meetups to share side-effect strategies.
- Attend virtual workshops on clinical trials, financial aid, and caregiving.
- Pair with a mentor who has navigated staging, surgery, or chemo.
Community voices also highlight barriers that can delay evaluation—like time off work or limited transportation—and teach ways to advocate for timely screening and follow-up. That collective experience can steady you as you plan next steps.
Raising Awareness and Education

Community education turns knowledge into action. Clear messages about colon cancer warning signs and the value of colon cancer screening help people spot changes early and seek care without delay. Outreach works best when it normalizes conversation and removes stigma.
Community Outreach Programs
Local campaigns can make a difference in neighborhoods, workplaces, and faith communities. Short talks at health fairs, employer lunch-and-learns, and mobile clinics encourage questions and build trust.
- Normalize discussion of bowel habit changes and rectal bleeding to reduce silence and fear.
- Highlight that symptoms lasting more than two weeks deserve testing and follow-up.
- Underscore that colon cancer screening starting at age 45 can prevent cancer by finding and removing polyps.
- Address unique barriers faced by women, who may be told symptoms are due to stress or anemia alone.
- Offer bilingual materials and on-site scheduling to turn intent into appointments.
Practical reminders—bring a symptom diary, know your family history, and ask about FIT, FOBT, and colonoscopy—help you advocate for timely care.
Available Educational Materials
Readers trust resources with clear language and medical rigor. Evidence-based guides from the American Cancer Society, the National Cancer Institute PDQ, the National Comprehensive Cancer Network, and Mayo Clinic explain what to watch for and what tests to expect.
- Symptom checklists: bowel changes, blood in stool, abdominal pain or cramping, gas or bloating, fatigue from anemia, weight loss, and a feeling of incomplete evacuation.
- Testing overviews: how FIT and FOBT detect hidden blood, why colonoscopy finds and removes polyps, and when imaging may be used.
- Action steps: track persistent symptoms, request evaluation if issues continue beyond two weeks, and ask about age-appropriate colon cancer screening.
- Women-focused notes: advocate if symptoms are downplayed; seek a second opinion when concerns persist.
Clear, concise materials empower families to recognize colon cancer warning signs and take the next step toward colon cancer screening without hesitation.
Conclusion: Staying Informed
Staying informed turns concern into action. Recognizing early signs of colon cancer and understanding common colon cancer symptoms helps you act sooner, not later. Small changes add up when tracked with care and shared with your clinician.
Importance of Ongoing Monitoring
Watch for shifts in bowel habits, blood in the stool—visible or occult—abdominal discomfort, persistent bloating, fatigue or weakness, and weight changes. The American Cancer Society notes that iron-deficiency anemia can be the first detectable sign; routine blood work and timely stool testing may reveal hidden bleeding before other cues appear. Keep simple notes. If patterns persist, that record speeds the next step.
Being Proactive About Health
Follow screening guidance starting at age 45 for average risk, and earlier if you have a family history, inflammatory bowel disease, or a hereditary syndrome. Adopt habits that lower risk, as advised by Mayo Clinic: eat a fiber-rich diet, limit alcohol, avoid tobacco, stay active most days, and maintain a healthy weight. If symptoms last beyond two weeks or worsen despite these steps, seek evaluation—women, in particular, face higher odds of delayed recognition. Early action can lead to polyp removal, curative surgery, and better outcomes. Know the early signs of colon cancer, stay alert to colon cancer symptoms, and partner with your care team for timely prevention and treatment.